By Sarah Lippert
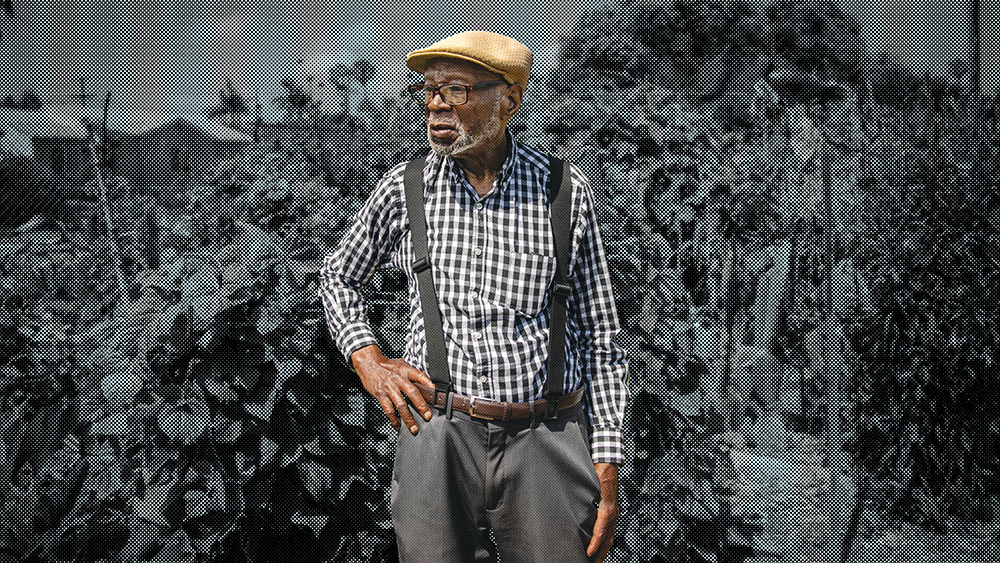
In 2022, people age 65 and older represented 17% of the American population. By 2040, that number is expected to grow to 22%, or 78 million Americans. Addressing the needs of older Americans means more than just studying the hospitals and long-term care facilities that serve them; it also means including their families and caregivers as part of the process. Ironically, one facet is often overlooked: patients’ individual opinions and wishes.
“As people age, they often feel like everyone wants to make the decisions for them and no one wants to listen to them. They feel disrespected because they move, talk, or process things more slowly,” says Karen Donelan, Stuart H. Altman Chair in U.S. Health Policy at Heller. “The majority of people served by our health care systems and hospitals are older adults, but they’re largely cared for by people who are younger.”
Donelan, along with Heller researchers Jennifer Perloff, PhD’06, and Carie Michael, and a team of experts and graduate students, is co-directing two multiyear studies at Brandeis funded by the Washington, D.C.-based Patient-Centered Outcomes Research Institute.
The first study, the Evaluating Novel Healthcare Approaches to Nurturing and Caring for Hospitalized Elders (ENHANCE) trial, led by researchers at Hebrew SeniorLife and the University of Michigan, began in March 2023. It introduces an additional element to engaging families and caregivers in the prevention and treatment of delirium, a sudden change in mental status marked by confusion and lack of awareness of one’s surroundings, commonly experienced by older adults. ENHANCE compares the standard implementation of the Hospital Elder Life Program, an effective and established clinical protocol whose overall goal is to prevent falls, shorten hospital stays, and decrease the need for nursing home care after discharge, with an adapted version in which family members and caregivers help to implement some of the program’s components.
“The study will be introducing more structure during family and caregiver visits,” says Donelan. “In terms of outcomes, we are measuring both the symptoms of delirium in the patient and the caregiver’s experience.”
The second study, Supporting Practices in Respecting Elders (SPIRE), is a collaboration with Massachusetts General Hospital, and takes a comparative look at what happens when an intervention is introduced to an existing primary care delivery model for older adults. SPIRE will partner with accountable care organizations’ primary care practices across the country to evaluate the impact of adding the Geriatric Resources for Assessment and Care of Elders model to Medicare annual wellness visits, including at-home assessments by nurse practitioners and social workers.
In keeping with the idea of improving results for those giving and receiving care, SPIRE will not only measure patient-related outcomes, like preventing hospitalizations and enhancing the patient experience in primary care, but also include surveying caregivers and primary care practices to assess whether the at-home model decreases the overall strain placed on caregivers in the medical system.
“We are consciously embedding these studies within systems and engaging all the players who have a stake in the outcome. When you include people in the conversation, you’re already having an impact,” Donelan says.
Research staff members work with stakeholders throughout both studies — allowing for real-time adjustments to improve processes — to provide support, particularly for patients and caregivers, to be heard, seen, and understood. The national SPIRE team will meet in late 2024 on the Brandeis campus to share their findings.
Donelan and her team hope for the outcomes of ENHANCE and SPIRE to reach far beyond gathering data and interpreting it; ultimately, she believes that “health policy needs to follow our humanity, not the other way around.”
