Authors: Renee Ferrari (UNC Chapel Hill), Hebatallah Naim Ali (Relational Coordination Analytics), Dina Alabsew (UNC Chapel Hill), and Lindsay Stradtman (UNC Chapel Hill)
Purpose: This study aims to explore barriers and facilitators to relational coordination between North Carolina’s CHCs and their referral endoscopy practices. The goal is to identify strengths and opportunities for ensuring quality follow-up for patients with abnormal CRC screening results. We also aim to assess the strength of internal coordination among the different roles within the CHCs. Then, test If internal coordination reflects on the strength of coordination with referral endoscopy practices. This will help determine if well-coordinated CHCs are more effective in managing and following up with their patients during the referral process than CHCs with low internal coordination.
Background: Colorectal cancer (CRC) screening with stool-based tests such as fecal immunochemical tests (FIT) necessitates specialty follow-up with a colonoscopy after abnormal results (FIT+). Delayed colonoscopy (>6mos) following a FIT+ is associated with increased risk of colorectal cancer diagnosis and late-stage diagnosis. Community health centers (CHCs) have a mission to serve patients with limited resources, including populations without health insurance. CHC patients commonly face multilevel barriers to screening completion and, unsurprisingly, CRC screening rates at CHCs are suboptimal. Ensuring timely, closed-loop patient care in the FIT+ follow-up process requires good communication and coordination between CHCs and referral endoscopy practices. Unfortunately, CHCs commonly report difficulties finding local endoscopy providers, obtaining timely appointments for patients, and receiving prompt colonoscopy results. Endoscopy practices also report issues such as CHC-referred patients missing their consult and colonoscopy appointments or arriving with poor bowel preparation. This highlights that miscommunication and failures to follow up intensify the coordination challenges. Identifying and addressing these issues is critical to enhancing patient care, increasing screening success rates, and reducing both the time and financial costs associated with CRC screening.
Methods: We propose to use Appreciative Inquiry and Relational Coordination (RC) frameworks to guide our exploration of linkages between North Carolina CHCs and the endoscopy practices to which they refer FIT+ patients. Appreciative inquiry is an approach to organizational change focused on core values and strengths, inspiring visions of an ideal future and encouraging contemplation on the path to achieving it. The RC framework will aid in understanding how staff within each organization, and across organizations, work together to achieve the goal of CRC screening completion with colonoscopy after a FIT+. Specific aims include: 1) Identify gaps in care coordination in the FIT+ to colonoscopy process in diverse, vulnerable populations; and 2) produce a prototype intervention in collaboration with a subset of CHC-endoscopy practice dyads for implementation with community partners.
Participants will be recruited from North Carolina’s 40 Federally Qualified Health Centers (FQHCs) and their associated referral endoscopy practices. We plan to administer a brief relational coordination survey followed by interviews with a subset of participants and site visits with CHC-endoscopy practice dyads who indicate interest in a relational coordination intervention.
Significance: Our work has the potential to address a common, intransigent weak link in the colorectal cancer screening care continuum, identifying and overcoming health system barriers to improve quality of care for populations facing barriers to health care.
Authors: Rachel Ross (UC Berkeley), Hector P. Rodriquez (UC Berkeley), Emmeline Chuang (UC Berkeley), and Stephen M. Shortell (UC Berkeley)
Project Summary: Patient-sharing clinician network configurations may serve as structural antecedents to relational coordination patterns among clinicians. The present work employs novel social network analysis to examine the association between Federally Qualified Health Center (FQHC) clinicians’ brokerage capacity and the management of hypertension and diabetes control among their patients. The sharing of patients between two clinicians, often across organizational or professional silos, frequently involves shared viewing or entering of electronic health record (EHR) data and/or discussing information about individual patients. From such interactions, evidence about the flow of information within network structures can be generated. Specifically, the present work examines the network construct of “brokerage,” which assesses the degree to which an individual may serve as a bridge between otherwise disconnected groups.
Context: The ability for clinicians to meaningfully interact and transfer information is essential to providing high-quality, patient-centered care for chronic conditions. This is especially true for FQHC patients who are socioeconomically vulnerable, have greater health-related social needs, worse control of chronic conditions, and experience more fragmented care compared to non-FQHC patients.
Methods: Patient-sharing clinician networks were constructed from EHR data from 38,298 patients seen by 664 unique providers across FQHCs in California that are members of the OCHIN Collaborative. Betweenness centrality scores were calculated for each clinician to determine clinicians’ brokerage capacity; mean betweenness centrality was then aggregated for each provider type present in our dataset (e.g., primary care clinicians, advanced practice clinicians, medical assistants, etc.). Regression models with facility fixed effects estimated the relationship between clinicians’ betweenness centrality scores and aggregated quality of care performance for A1c control and systolic and diastolic blood pressure management.
Key Findings: Measures of brokerage capacity did not vary meaningfully across the clinician roles included in our data. Higher betweenness centrality among primary care clinicians was associated with slightly better A1c control. However, no significant associations between brokerage and blood pressure outcomes were found, suggesting that the benefits of brokerage may vary by the complexity of condition management or other unmeasured aspects of interaction, such as the frequency or quality of communications.
Discussion: In summary, our findings may reflect an overall network structure in which few “holes” in communication existed for clinicians to bridge. The association between betweenness centrality and A1c control among primary care clinicians supports the notion that certain brokers may indeed facilitate information and resource flow across network gaps, and therefore enhance complex chronic disease management efforts. Importantly, relational coordination may manifest as FQHC clinicians engaging in informal conversations to share best practices, or as managing interdependent tasks required for successful patient care (e.g., health education efforts or follow-up calls) that may not be captured as formal encounters in an EHR. Therefore, future research should build on this foundation of evidence by integrating more granular information about patient encounters and care team structures, to enable a deeper understanding how diverse network structures can improve care for chronic conditions by shaping interactions and promoting relational coordination mechanisms.
Authors: Brenda Reiss-Brennan (Intermountain Healthcare System), Stephen M. Shortell (UC Berkeley), Chad Boult (Centers for Medicaid and Medicare Services), Mariko Carey (University of Newcastle), Aine Carroll (University College Dublin), Nick Goodwin (University of Newcastle), Zoi Tirandafilidis (University of Newcastle), and Jason Yap (National University of Singapore)
Summary: Building on Complex Adaptive Systems (CAS) concepts, we propose an overarching social science framework for addressing the fragmentation that exists in health and social care systems worldwide. We focus on how relational networks might be strengthened to deliver more coordinated, integrated person-centered care. The framework is used to examine a major emerging social experiment in New South Wales, Australia: All-Inclusive Care for the Elderly" ( ALICE ).
Context: Existing research on integrated care has largely focused on structural elements of care with mixed results (Goodwin, 2004; Burns et al., 2022). This approach has largely ignored the complex, emergent, ever-changing relational dynamics of how care is delivered. To address this gap, we merge social network theory (Granovetter, 1973; Kadushin, 2022) and relational network theory, (Gittell and Weiss, 2004) to develop a relational network theory that addresses the complex ecosystem of health and social care delivery. Network ties involving strength, centrality, density, embeddedness, and structural holes are made "social" by the extent to which the network actors share common goals, trust, mutual respect, and engage in frequent, specific, accurate, and problem-focused communication. These relational processes both influence and are influenced by the structural network properties and impact outcomes.
Methods: ALICE is an emerging community-based relational model of care for older people on the central coast of New South Wales. Traditionally, healthcare for older people has been complex, fragmented, and not focused on social needs. The Relational Network Theory (RNT) framework highlights three core principles of ALICE: 1) the promotion of "link workers" who conduct holistic assessments and coordinate access to care across caregivers; 2) the development of integrated care communities that leverage social connections and networks through use of kiosks and community engagement officers to support older person care; and 3) a commitment to healthy "place-making" with local governance and engagement forums to create healthy built and natural environments to support older people in living healthy and active lives.
Findings: The ALICE initiative has been co-designed with residents and stakeholders from different sectors to implement an agile approach that will work in different community settings and contexts. This is a foundational step in spreading and scaling outcomes. The relational work in creating new roles (linkage staff and engagement officers) is building the required connections and trust to meet the whole-person needs of older people. A key finding is the need to assess and map the complex social and relational network properties carefully to facilitate successful spread and sustainability. Two important recommendations for policymakers, providers and managers are to: 1) recognize health and social care delivery as a Complex Adaptive System (CAS) with all of its' implications; and 2) co-design new care models following the framework of (RNT) building in social reciprocity among all actors to reduce the current fragmentation and advance more socially connected care.
Authors: Scott Soltis (University of Kentucky) and Al-Karim Samnani (University of Windsor)
There has been increased attention to the importance of workplace relationships in facilitating employee and organizational success via human resource management. This has led researchers to explore several distinct, but related concepts and theories, such as relational climate, relational coordination, and social networks.
Building upon the strengths of each perspective, this manuscript develops an integrative relational theory. The integration of multiple relational mechanisms at the individual- and group-level advances our understanding of the role of social capital in human resource management.
By enriching our view of relational environments via an integrated theory, synergies emerge allowing for a greater understanding of 1) how employees fit within the collective process (i.e., shared relational context), 2) the gathering and sharing of diverse information from cross-functional interdependent ties, 3) the meaning of engagement in high-quality and frequent communication within their units, and 4) the development of expressive ties with organizational members which extend beyond task interdependencies. The criticality of this model for an accurate understanding of relational environments in HR is demonstrated via a variety of HR applications.
Authors: Jim Best (Independent Consultant) and Lauren Hajjar (Suffolk University)
In a world facing wicked social challenges such as pandemics, authoritarianism, social injustice, and climate change, calls for holistic responses are increasing. Addressing complex social challenges requires the collaboration of multiple and simultaneous relationships across multiple levels. Management scholars have explored how organizations and communities effectively prepare for, respond to, and overcome various degrees of challenges. Yet, there is a need to further understand how to develop resilience in response to adversity and also as an opportunity for future growth.Resilience, as a multilevel process, enables individuals and their systems to not only withstand but also to thrive in the face of adversity. At all systems levels adverse impacts may be successfully absorbed with or without essential internal changes. Although there are other important types of resilience we might address, in this session we’ll focus on resilience to adverse impacts. A key mechanism for fostering resilience is the availability of slack resources, including relationships.As scholars and practitioners we hold a good deal of wisdom about designing resilient relational practices and work systems. Can we harvest that together?
This group session is an interactive experience exploring relational practices and work systems enacted at multiple levels that strengthen resilience. We offer a resiliency landscape to anchor the three short presentations that, together, provide a context for rich and mediated small and full group discussions. Collectively we’ll explore relational practices and work systems we’ve encountered in practice or in the literature that provide insights into designing for resilience.
Author: Sarah Phillips (Pretrial Services Coordinator, St. Louis)
The St. Louis pretrial services program aims to bolster judicial decision-making within the 22nd Judicial Circuit by enhancing pretrial services and building resilience within its operational framework. Initially challenged by limited functionality and staffing shortages, the Pre-Trial Release Office (PTR) lacked robust case management capabilities. This program, which began in 2021, was designed to address these shortcomings through collaborative partnerships and the implementation of an innovative pretrial services model. Central to the program's strategy was the establishment of collaborative partnerships with stakeholders including the Missouri State Public Defenders Office, community service providers, and multiple justice system agencies. These partnerships were intended to streamline defendant support services and enhance data feedback to the courts. Specific activities included formalizing alliances with service providers for in-jail outreach and seamless transitions to community-based services, alongside the adoption of advanced pretrial case management software. Resilience-building efforts within the pretrial services were based on relational coordination survey results and included structured meetings and huddles, specialized training sessions, warm hand-offs with clients, and ongoing communication with judges, attorneys, and community partners.
Process and outcome evaluation data between 2020-2024 reveal increased judicial confidence in bond decisions and high participant court appearances. Results also show a reduction in re-arrest rates and favorable case resolutions, while long-term objectives remain focused on lowering recidivism through strong participant-caseworker relationships and community interventions. Despite challenges in data tracking, findings demonstrated promising participant engagement and positive court outcomes, indicating potential long-term benefits for criminal justice practices within the circuit. Collectively, the structures, processes and relational practices implemented in the 22nd Judicial Circuit Court reflect an innovative approach to pretrial service delivery and offer a promising model that may improve defendant outcomes and enhance judicial efficiency.
Author: Erik Nicholson (Pandion Strategy)
This case study illustrates resilience in action within the agricultural sector, navigating adversity through collaborative governance and proactive safety measures, thereby shaping long-term impacts on worker well-being and industry standards. As the pandemic unfolded across the United States, the essential role of agricultural workers in food production became evident. For many of us who’ve worked on the labor side of agriculture, this recognition was long overdue and welcome. However, it quickly evolved into an unsafe work environment as farm workers faced significant health risks associated with minimal protective measures such as social distancing and access to hygiene facilities. These essential workers were now expected to continue working in the fields while many other working people were able to more safely shelter in place.
Despite federal and state-level agency calls for social distancing, frequent handwashing and masking, none of these measures were widely adopted on farms. Workers continued to work in close proximity to one another, handwashing facilities continued to be a quarter mile away from workers (more than four football fields in distance) and the only masks available were the ones workers may bring from home. Workers received no updates or information about the pandemic and their places of employment. Reports revealed that entire crews would one day from the next disappear with no explanation. Growers privately shared that the food supply chain was at times 2-3 days away from complete collapse. Neither the state nor federal government had stepped in to issue binding regulations. Therefore, a third option was needed.
Drawing on pre-existing relationships, sometimes cordial, sometimes adversarial, the United Farm Workers and grower trade groups came together to develop a draft set of rules they would ask the State to adopt. They embraced a mission statement that upheld protecting essential workers employed in agriculture from COVID 19, while ensuring the continuity of the supply chain. This initiative culminated in the adoption of pioneering state regulations in Washington, establishing a precedent for workplace improvements. Enhanced proximity of hygiene facilities and heightened awareness of health impacts underscore a shift towards resilience-building practices. Today, agricultural workers, supported by ongoing advocacy, continue to assert their essential status amidst prevailing anti-worker sentiments in the United States. The presenter, lead negotiator from the United Farm Workers, remains actively engaged in advancing these efforts.
Author: Wale Olaleye (Deloitte Human Capital and RC Analytics)
This case outlines how a Hospital Health Network (HHN) in Ontario responded to COVID-19 challenges by implementing strategic interventions at individual, organizational, and systemic levels. These efforts aimed to strengthen communication and resilience and establish flexible staffing models and partnerships to improve crisis response, reduce burnout, and optimize resource utilization, serving as a model for enhancing healthcare system resilience globally. A Hospital Health Network (HHN) in Ontario, like many health systems across the world, faced significant challenges during the COVID-19 pandemic, revealing weaknesses in emergency preparedness and other operational processes.
To address some of these issues, the HHN implemented strategic interventions to enhance resilience at individual, organizational, and systemic levels. The objective of these efforts was to transform vulnerabilities into strengths, ensuring the system's ability to adapt and thrive in future crises. HHN improved communication by strengthening collaboration between interdisciplinary teams and adopting digital communication platforms. Organizational structures implemented include training programs, proactive monitoring, and feedback loops, helping healthcare workers stay focused and responsive. These practices fostered a culture of continuous improvement and awareness. In response to surges in demand, the HHN developed flexible staffing models, maintained reserve supplies, and established partnerships for resource sharing. These measures ensured that personnel and essential medical supplies could be quickly reallocated as needed. They also strengthened community health networks, regular knowledge-sharing sessions, and an integrated electronic health record (EHR) system.
The outcomes of these efforts included improved crisis response, reduced burnout and higher job satisfaction among healthcare workers, efficient resource utilization, and enhanced continuity of care. HHN’s resilience-building strategies provide a model for other health systems, demonstrating how coordinated, mindful, and flexible approaches can transform challenges into opportunities for growth and adaptation.
Author: Steven Tizio (Riverview Medical Center)
Context. Riverview Medical Center in Red Bank, New Jersey is a community hospital and part of the Hackensack Meridian Health System. Since the COVID-19 pandemic, there appears to be a deterioration in the doctor/nurse relationship in the Medical/Surgical Unit. Riverview has an online reporting system “ONELINK” whose goal is reporting clinical issues for quality improvement. This would be part of a “great catch” system where providers felt safe reporting errors to improve patient care. Lately, if there is a disagreement between a physician and nurse, a ONELINK is filed – there is an increase in reports of “workplace violence” or “workplace hostility” – there is an increase in reporting providers to this anonymous system which is leading to a deterioration in the doctor/nurse relationship. The reporting system is inaccurate and appears to be more focused on “finger pointing” than problem solving.
Methods. In Summer 2024, the Vice Chair of Surgery proposed to use relational coordination principles and methods to revitalize the doctor/nurse relationship and to end this hostility in the interests of better patient care. The first step was to create a change team of key stakeholders. Secondly, to analyze the current state with the change team using two tools - relational mapping analysis and organizational structures assessment. And thirdly, to propose interventions to strengthen organizational structures, relational coordination and desired performance outcomes.
Findings. The Vice Chair succeeded in engaging key stakeholders as part of the change team. From the relational map they learned there are many interactions with the patient on the Med/Surg floor. The Doctor, Nurse, and Patient have the best relational coordination (the patient is central), yet RC is not optimized with the doctor and nurse. Doctors and Nurses have competing goals, exclusive knowledge, and the mutual respect has deteriorated. Infection Control and the Patient Experience Department are part of the larger hospital system and they tend to have poor RC with each other. The Case Manager was designed to be a boundary spanner role, but no longer plays this role, and their relationship is strained with all the caregivers. The Patient Care Technician appears to have the best RC on the floor. They may be more vital to the care team than realized by most providers. Using the Org Structures Assessment Tool, the team assessed that every role receives training for teamwork, that every role uses the Epic system to write notes and receive patient information, and that Nurses have a daily huddle. Providers share space on the floor for documentation, which allows for real-time communication. On the negative side, there is no shared accountability, there is currently no boundary spanner role, the existing conflict resolution process supports passive confrontation, there are minimal shared rewards, and Doctors are not part of Nurse huddles.
Next steps. The following interventions have been proposed with more refinement needed. Doctors should be part of the nurse floor huddles. There should be a structure that enables shared accountability, given that doctors and nurses have different systems to manage quality, leading the two parties to appear misaligned. Should doctors and nurses be the new boundary spanner in the hospital? There are no shared rewards – there is profit sharing for the doctors, but no incentive to improve RC with the nursing staff. Recommend increased use of shared protocols, such as Enhanced Recovery After Surgery,which already include most roles on the team.
Author: Yamini Howe (Cortica)
Context. Autism is a neurobiologically complex and highly heterogeneous condition. Autistic individuals often require highly specialized care from across disciplines, which is costly. Furthermore, care is highly fragmented, and there is a shortage of medical, behavioral, and developmental providers across the country. To address the need for cost-effective whole-child care across disciplines, the healthcare startup Cortica was carefully designed to bring together a team of outpatient providers under one roof: Medical (MDs, Medical Assistants, EEG technicians), Developmental Therapists (Speech-Language Pathologists, Occupational Therapists, Music Therapists), and Behavioral Specialists (ABA). The startup began with an initial clinic in San Diego and has expanded across the country. A Whole Child Score Card metric was piloted by the Cortica team in order to monitor care of autistic children served by the Cortica multidisciplinary team. Initial research has shown that receiving care within the Cortica clinical model can lead to improvements in the adaptive functioning and quality of life of the child. At our newly established Cortica site in Burlington, MA, we are leading the company in innovating a value-based care model to provide care at a multidisciplinary clinic, using the Whole Child Score Card as our outcome measure.
Method. This descriptive case presentation is a work in progress. We will describe the implementation of relational and structural interventions in the context of Cortica Burlington. Interventions such as engaging in humble inquiry, relational mapping, and creating psychological safety that were utilized in the initial phases of team development, with subsequent adaptation of the Cortica Medical Rounds model to become cross-disciplinary rounds.
Findings. Using relational theory, we have set up the basics of the key clinical team and relationships, leading to successful expansion, growth of the center, and high patient satisfaction, but a high degree of instability in staff retention remains. An initial relational coordination map indicated the team is heading towards silo development, with little cross-disciplinary communication and with significant communication challenges.
Next steps. Over the next few months, our team hopes to examine how the local team builds while implementing the new Whole Child Score Card at Cortica Burlington, and examine how relationship dynamics affect functioning of the team, thereby setting the clinic up for long-term success in providing well-integrated, holistic, potentially transformative autism care, that eventually leads to demonstrable quality of life improvements on the Whole Child Score Card.
Author: Jennifer Pope (Department of Emergency Medicine, Dartmouth Hitchcock Medical Center)
Context. Older adults engage with the healthcare system across many touch points, perhaps none as frequently as the ED. 29 million annual ED visits were made by patients age 60 or older (2014-2017). 60% of avoidable hospital admissions are for patients 65 and older. At Dartmouth Hitchcock, for elderly patients who do not have a medical reason for hospital admission, we have an ED fragility observation protocol which means elderly patients stay overnight in the ED to be seen by physical therapy (PT), case management (CM), the Geriatric RN, and social work (SW) to determine the resources needed to get them home safely. Patient and family often expect that our team can get them into a nursing home or find some service to care for them in the home immediately even when the patient’s decline has been going on for some time.
Methods. In Summer 2024, a physician leader proposed to use relational coordination principles and methods to strengthen the coordination of this work process for elderly patients in the ED. The first step was to create a change team of key stakeholders. Secondly, to analyze the current state with the change team using two tools - relational mapping analysis and organizational structures assessment. And thirdly, to propose interventions to strengthen organizational structures, relational coordination and desired performance outcomes.
Findings. The physician leader and the change team discovered that RC works well in several areas: The relationship between the CM, Geriatric RN, and SW with the patient and families is excellent. They have the time to connect with the family and get a better understanding of immediate physical and psychosocial needs. In addition, the PT assessment is incredibly helpful to determine the patient’s actual needs, identify missed medical issues, and provide patients and families with encouragement around what patients can actually do with assistance like a walker. They also discovered that RC works poorly in several areas: The ED RN is pulled in many directions and often cannot provide specialized geriatric care which can result in patients declining in terms of mobility. Families often will be upset with the ED MD/APP if we do not admit the patient to the hospital. They do not understand that if there is no medical reason for admission that we cannot admit the patient. Even if the ED MD/APP thinks a patient is unsafe to go home, the CM and SW often have to find the next safest option because it is difficult to place people directly into assisted living or nursing homes. We have Geriatric RNs who work with patients and families but in this exercise, we discovered that the ED MD/APPs and ED RNs do not really know what they do or when they assess patients to share feedback and concerns. Currently, ED MD/APP and ED RN engagement with the fragility protocol is somewhat negative because the communication is often disjointed and resulting in frustrations from patients and families due to unrealistic expectations and limited outpatient resources.
Next steps. An organizational structures assessment has also been conducted and results will be shared. As a team, we have opportunities for improved communication in order to improve patient care and outcomes. Our biggest opportunities for change, at this point in the analysis, appear to be understanding the role of the Geriatric RN, and improving the upfront communication with patients and families about expectations for placement, home services, and ultimately, in most cases, getting the patient back to their home environment.
Author: Mariko Kita (Virginia Mason Franciscan Health)
Context. The Pulmonary Clinic team at our Federal Way campus successfully engaged in very challenging but critical work in navigating vulnerable, difficult conversations to establish expectations for respectful behaviors in the workplace in March 2024. A physician leader invited them to participate in further improvements using Relational Coordination methods. The team selected the process of successful scheduling of referrals from both internal and external referral sources which includes the appropriateness of scheduling, the collection of outside records and imaging as well as handling and reducing no-shows.
Methods. Using relational coordination principles and methods to strengthen coordination of the work process for referrals and access to the pulmonary clinic, the first step was to create a change team of key stakeholders. Secondly, to analyze the current state with the change team using two tools - relational mapping analysis and organizational structures assessment. And thirdly, to propose interventions to strengthen organizational structures, relational coordination and desired performance outcomes.
Findings. We learned that prior team-building work done in March 2024 had paid off, with the core clinic team reporting that RC was strongest within the core roles of the clinic and also between internal referring providers and clinic team members. RC was not working well however in the external processes especially with The Access Center and the Clinic where shared goals were at odds with each other. Communication was poor between Access and Radiology where studies will need to be performed or collected, there was a lack of problem-solving behaviors between imaging, clinic and Access Center, and no consistent way to reach outside referral sources. The impacts of poor relational coordination on performance were manifold resulting in disappointment with the encounter, waste and delay in medical care, missed opportunities to provide our patients the best expertise and repetition of mistakes. Some of the existing organizational structures were assessed to be consistently supportive of relational coordination including shared information systems, selection for teamwork and training for teamwork and within the core team, shared accountability, shared meetings, shared protocols, shared space. Moderately well supported structures included conflict resolution. As an overarching observation, the outside referral source structure was deemed to have inherently poor support for relational coordination. Despite consistently strong support for selecting for teamwork across every role, a striking observation was the poor support in terms of job design: “It seems like it is expected that the job will accomplish coordination, but the job is not designed to execute coordination!”
Next steps. In sum, there have been several proposed solutions thus far. The team called out a desire for a boundary spanner in the form of a referral coordinator and other ideas included sharing a folder to make a pre-appointment checklist visible; revising the scheduling guide for better accuracy in appointing; a feedback loop to the Access team to call out opportunities or successes. The team called out the desire to have someone from the Access team and Imaging as part of the change team. These proposed solutions will be further refined before the Roundtable in November.
Authors: Ina M. Sebastian (MIT CISR), Thomas Haskamp (University Münster), and Helen Saar (Utah Tech)
In 2023, we studied how companies govern digitally enabled ecosystems. We have conducted fifty interviews with executives and Web3 experts from fifteen countries in 2023 and 2024. Industries included healthcare (e.g., health system Kaiser Permanente), financial services, manufacturing, agriculture, ocean shipping, automotive, information technology, and government. In our interviews, we identified three types of ecosystem governance—alpha (single leader), representative, and liquid (Web3-enabled decentralized)—that enable companies to successfully pursue business strategies within ecosystems if governance aligns with how ecosystem participants expect to interact (Benedict & Sebastian, 2024).
In another research project, we studied how technology leaders help their companies scale carbon emission reduction. We hosted a discussion with 36 executives of the MIT CISR Data Research Advisory Board and have conducted 37 interviews with 40 executives from ten countries in industries including healthcare (e.g., health plan Bupa), pharma, financial services, manufacturing, agriculture, supply chains, automotive, high tech, and government. Reducing carbon emissions requires that technology leaders consolidate data about their company’s carbon emissions, combine it with data from their suppliers, partners, and customers, and make the data available to and actionable by the company. For maximum impact on the shared problem of carbon emission reduction, transparency should extend all the way to end consumers.
In our study, technology leaders worked to build a tracking capability that relies on digital technologies and accurate, granular data. They were using this capability to pursue three opportunities, each with a focus on reducing Scope 3 emissions - those by the company's suppliers, partners, and customers (Greenhouse Gas Protocol) - through digitally enabled ecosystems: 1) Replacing carbon-intensive technologies, 2) Decarbonizing products, and 3) Creating digital offerings to track and optimize emissions for suppliers, partners, and customers (Sebastian, Haskamp, & Woerner, 2024). Both research projects are ongoing. We study what the essential elements are for an ecosystem to be healthy and how organizations architect successful ecosystem collaboration through effective governance and other elements, including digital platforms.
In this presentation, we provide evidence of the value of digital and data capabilities for healthcare organizations and emerging healthcare ecosystems, discuss how organizations can measure digital value, and explore design options for digital and data capabilities at the ecosystem level. We illuminate value from the information systems, relational perspective, and finance perspectives. We hope to address the question of whether and how digital and data capabilities should be part of the certifications of healthcare providers and health plans under the proposed Better Care Plan. We will draw on the example of Kaiser Permanente. The organization has developed a value dashboard that tracks value from digital for patient care and is used by the leadership team and customer experience teams (Woerner, Weill, & Sebastian, 2022), it extends its value-based care model, including digital and data capabilities, to community-based, multi-provider, multi-payer health systems through Risant Health (Forbes, 2023), and it was a founding member of Graphite Health, launched by 4 health systems with the goal of “a common digital language for health.
Author: Elizabeth Davidson (University of Hawaii)
Ubiquitous digitization of socioeconomic transactions, proliferation of user content via social media and Internet use, adoption of mobile consumer applications and digital devices that record intimate human activities, and the rollout of IoT devices - all contribute to ever-growing stockpiles of digital data within and across organizations (and their technology infrastructures) (Gregory et al., 2021). These data resources have the potential to address grand challenges by enabling innovations that improve the quality and sustainability of human lives and societies (Davidson et. al, 2023). Through monetization and innovation, they also generate untold profits and economic influence for the firms that control these resources (Zuboff, 2015).
Reuse (and misuse) of data in new contexts and for new purposes, particularly when coupled with advanced technologies such as generative AI and machine learning, have the potential to improve societal wellbeing but also to degrade it, for instance by invading individuals’ privacy, usurping their autonomy, and contributing to bias and discrimination (Murdoch, 2021; Winter & Davidson, 2022).
Ethical approaches to data governance policies and practices within and across organizations, guided by meaningful societal regulation, are essential to balance social, economic, and technical benefits with potential harms for individuals, organizations, and societies.
Health systems need to share highly sensitive data for patient care and for research and health system innovation, and several exemplary data management practices have developed in healthcare. Based on her long-term study of organizations that serve as stewards of various types of healthcare system data, and their goals of sharing data more broadly and effectively, Liz will explore emerging health data ecosystem infrastructures with consideration for ethical approaches to data governance. Of note, new "data space" legislation in the EU is meant to enable the sharing of health data for clinical purposes and innovation across the EU (European Commission).
Similarly, the U.S. Office of the National Coordinator (ONC) recently released a comprehensive framework to enable health data exchange among clinicians, researchers, patients, and so on, termed the Trusted Exchange Framework and Common AgreementTM(TEFCATM). These frameworks aim to facilitate nation-wide health data governance capabilities to deliver on the promises of earlier, fragmented health information exchange efforts. There are many factors inherent with inter-organizational data sharing and collaborative efforts in healthcare that give rise to such novel health data governance structures but also challenge their effective operation, including differences in goals and constraints (even among actors we would think are cooperative like state agencies) and regulatory limitations.
A key finding of researchers and practitioners working to facilitate comprehensive health data resources and exchange is that ‘data moves at the speed of trust.’ Trust is critical in building and maintaining relationships for data exchange and experience and knowledge sharing, particularly via collective actors (e.g., vendors but also not-for-profit facilitators). Shared goals and shared values - including ethical governance - developed through multiple communication channels are critically important to creating this trust.
The presenter will draw from her research on health data governance organizations to highlight exemplary data governance practices and techniques. She will explore the relationships between policy, purpose, innovation, and value in the creation and use of digital data resources, and explore approaches to embed effective ethical governance approaches into data management technologies, sociotechnical platforms, and organizational practices. She will highlight actions practitioners can take to “bake” ethical data management and governance into organizational and interorganizational technologies, practices, and strategies. She will explore opportunities for the Better Care Plan, whose third pillar seeks to establish national patient safety and health outcomes reporting.
Author: Tomaz Sedej (Hyperledger Foundation)
Building successful digitally enabled ecosystems requires more than technological prowess. It demands robust governance, sustainable business models, and effective operational execution. Hyperledger, an open-source project hosted by the Linux Foundation, exemplifies the importance of shared vision and collaborative governance. As digital ecosystems evolve, investing in co-innovation and ecosystem adoption is crucial.
As a PhD student at Copenhagen Business School, Tomaz Sedej studied the TradeLens global shipping platform, a compelling, emerging digitally enabled ecosystem that was shut down after 3 years. As an ecosystem manager at the Hyperledger Foundation, he is responsible for growing a not-for-profit digitally enabled ecosystem and understands the potential of decentralized Web3 technologies and convergence with AI. The current analysis includes a comprehensive review of 12 blockchain-enabled for-profit and not-for-profit ecosystems across multiple domains, including supply chain management, healthcare, and digital identity. The review includes governance mechanisms, business model sustainability, and operational execution challenges like interoperability and scalability. Case studies include TradeLens, We.Trade, GSBN, and LACChain.
Additionally, three healthcare ecosystems are analyzed, including Synaptic Health Alliance, a consortium that uses blockchain to improve healthcare provider data management, and the Vaccine Ledger, a solution backed by UNICEF that enhances the traceability and efficiency of vaccine distribution, demonstrating the practical benefits of blockchain in healthcare ecosystems. The cases illustrate that blockchain technology, initially recognized for its role in cryptocurrencies, now facilitates secure and confidential transactions among multiple entities in various domains, including healthcare.
However, a key finding of the research is that success of blockchain enabled ecosystems depends not only on technological capabilities but also on effective governance, viable business models, and operational execution.
Governance: Establishing clear and transparent governance mechanisms is crucial. TradeLens, a supply chain platform by Maersk and IBM, faced resistance due to centralized governance and data-sharing concerns. Despite involving multiple ocean carriers, governance issues led to its eventual shutdown. Conversely, the Global Shipping Business Network (GSBN) exemplifies successful governance with a collective decision-making process. Business Models: Blockchain ecosystems must offer clear value propositions. We.Trade, a trade finance platform backed by major banks, failed due to a lack of clear value for corporate clients. In contrast, LACChain, a non-profit public blockchain platform, provides a neutral and reliable infrastructure, fostering widespread adoption by offering clear value to its participants. Operational Execution: Successful projects must integrate with legacy systems and ensure seamless data flow. TradeLens faced difficulties with interoperability, particularly integrating with small local banks with outdated systems.
Effective digital ecosystems leverage relationships and communication to respond to uncertainty and support interdependence. Emerging ecosystems must focus on refining governance structures, developing clear value propositions, and enhancing operational interoperability to create resilient, collaborative environments capable of addressing complex challenges in healthcare and beyond.
Author: Yu Wang (Regeneron Pharmaceuticals, Inc.)
Context: In the pharmaceutical industry, data scientists play a crucial role in managing vast datasets, particularly in the oncology sector where timely and accurate information plays a vital role for patient outcomes. This abstract discusses how integrating relational coordination and advanced analytics can enhance drug commercialization efforts, specifically through artificial intelligence (AI) and machine learning (ML) technologies. Pharmaceutical companies traditionally operate in silos, with marketing, sales, pricing, market access, medical affairs, and health economics and outcomes research (HEOR) teams working independently. However, fostering collaboration across these functions and with external partners—such as payers, providers, and healthcare professionals—allows for a holistic view and the discovery of new methodologies and opportunities to improve patient care and operational productivity. Methods: Through dialogue and deep listening, we have aligned perspectives and coordinated efforts more effectively. For example, AI and ML technologies have been used to analyze diverse data sources, identify future trends, and predict patient outcomes, enabling the development of targeted strategies for oncology treatments. Our project shows that relational theories, methods, and practices, combined with advanced analytics, can significantly improve healthcare delivery.
Findings: This collaborative approach has led to several key outcomes: Improved Patient Outcomes: By integrating data from various stakeholders, we better understand patient needs and tailor treatments accordingly, resulting in more patients receiving appropriate and effective oncology therapies.
Increased Operational Productivity: Enhanced coordination and data-driven decision-making have streamlined operations, reduced redundancies, and improved efficiency across the drug commercialization process. Enhanced Stakeholder Engagement: Building strong relationships and networks among internal and external stakeholders has facilitated a cohesive approach to addressing complex challenges in oncology.
Implications: Collaborative efforts across internal functions and external partners are essential for identifying and addressing opportunities in oncology treatment. AI and ML technologies enhance the ability to analyze large datasets and develop targeted and effective treatment strategies. Improved coordination and stakeholder engagement lead to better patient outcomes and increased operational productivity.
Data Integration Workshops: Participants will engage in hands-on activities to explore methods for integrating diverse data sources and utilizing AI/ML technologies.
Relational Coordination Simulations: Attendees will participate in simulations to experience the benefits of deep listening and dialogue in fostering collaboration.
Case Study Discussions: Real-world case studies will be presented, followed by group discussions to identify best practices and lessons learned in relational coordination and advanced analytics. In summary, these initiatives foster a deeper understanding of how relational coordination and networks can transform the pharmaceutical industry, leading to better healthcare solutions for oncology patients. By viewing the whole together through relationships and advanced analytics, we can design solutions for complex challenges and engage in coordinated collective action for multilevel systems change.
Authors: Richard W. Stackman (University of San Francisco) and Zoe I. Barsness (University of Washington-Tacoma)
Our current research focuses on the need for a paradigmatic shift from the dominator (individualistic) paradigm to a partnership (collective) paradigm (see Riane Eisler and David Graeber & David Wengrow) where care and caregiving are at the forefront of society. The ability to pursue meaningful work and lives for optimal human development depends on caring and caregiving at the individual, organizational, societal, and environmental levels. This paradigmatic shift to a focus on care synthesizes the work of Eisler, Graeber and Wengrow, Jennifer Nedelsky, Elinor Ostrom, Claudia Goldin, Marvin Brown, and Kate Raworth, reinforcing a future built upon contributive justice (Michael Sandel) and inclusive prosperity (Sir Paul Collier).
Current (and dominant) models of business (neoliberalism) and management (agency theory) are deficient with respect to how we prioritize care and caregiving. In her book – A Paradise Built in Hell: The Extraordinary Communities that Arise in Disaster – Rebecca Solnit demonstrates how catastrophic events create opportunities for humans to unlock desires that had heretofore been unacted upon because of the existing social reality and institutional structures. Events such as earthquakes, terrorist attacks, hurricanes and the recent pandemic are punctuated equilibria that bring communities together and disrupt taken-for-granted norms and the embedded power structure. These events reveal the power of mutual aid, level the playing field for all and open avenues of opportunity for individual, organizational, and communal renegotiation and reinvention.
Many lessons have been learned and insights gained from the pandemic which encouraged us to question how human activity is structured and its impact on our well-being. None of these is more important than how we have prioritized work over care. During the pandemic, for example, employees whose only option was to work from home were able to reapportion their time, primarily around work and home care responsibilities, with the elimination of their daily commute to work. While the pandemic didn’t necessarily make the work-life balancing act easier, employees enjoyed greater flexibility and autonomy. Post-pandemic those who held power have unfortunately worked to recapture their authority as evidenced by the increasing number of return-to-office mandates and consequent curtailment of employees’ ability to work from home.
The re-emerging pre-pandemic forms of social organization will continue to inhibit our ability to nurture and foster human potential to the fullest by creating a sustainable “care society.” (We have purposely chosen to use “care society” instead of a “care economy.”) A “care society” prioritizes the care of all – especially the young, elderly, our communities, and our earth. Unfortunately, the dominant neoliberal perspective has nurtured a vulture capitalism. This vulture capitalism, with its drive toward financialization of all things, is undermining, among other things, self-care, health care, childcare, elder care and environmental care. This is unfortunate as capitalism is perhaps one of the most consequential ideas we have ever had, enabling untold human progress. Elevating a partnership paradigm to inform our conversations and research provides the opportunity for an interactive discourse at the Roundtable focused on the question: How can a caring sustainable society and capitalism co-exist?
Authors: Deborah Blackman (UNSW Canberra), Vindhya Weeratunga (UNSW Canberra), Emma Sparkes (UNSW Canberra) and Jo Chaffer (UNSW Canberra)
This presentation addresses issues related to breaking human resources activities into “manageable” subsystems. Theoretically the various HR activities of selection, recruitment, development and so on, are brought together via strategic HRM but, in reality, they often work separately, affecting the larger system in ways that either: emerge over time challenging ongoing decision making, or create unintended, potentially detrimental, consequences. Considering these challenges, we present a book project supporting the creation of high performance through applying relational and systems perspectives to strategic HRM concepts.
The philosophy of relationality emphasizes the interconnectedness and interdependence of entities. The focus is on the connections and interactions between things, rather than on the things themselves: Taking a relational orientation suggests that the real work of the human organization occurs within the space of interaction between its members. Thus the theorist must account for the relationships among, rather than the individual properties of, organizational members (Bradbury and Lichtenstein, 2000, p551).
In a relational worldview, all of the components of a system exist in relation to one another (Caves and de Melo, 2018). Any entity is defined as being in a relationship with something else, with these relationships creating identity and potentially new perspectives. Consequently, relationality suggests that an entity’s nature is determined by its relationships with others, rather than by its inherent qualities or properties; entities are not seen as discrete, self-contained objects, but rather as nodes in a network of relationships that constantly affect and shape each other.
So what happens if we link this to systems? Both relationality and systems thinking emphasize the interconnectedness of elements. A system is a configuration of stocks and flows and only by changing a flow can stocks change over time (Meadows, 2008), thereby leading to different system behaviours. Integrating relationality with systems thinking offers a useful lens through which we can understand and manage organisational dynamics, considering that it is not reconnecting HR activities that offers a way forward, but rather using strategic HRM to shape system outcomes through changing the system relationships.
Shared purpose, interdependencies and leverage points are discussed, considering if these systems perspectives offer a way to reframe strategic HRM. We will argue that using this lens to focus on the relational, agentic areas of intersection will support a perspective of seeing strategic HRM as shaping system movement rather than solely creating outputs and outcomes. This approach will be reflected in a book that offers people managers a different analysis of issues and alternative ways forward.
Authors: Qian Zhang (University of Ottawa, Telfer School of Management)
The field of human resource management (HRM) has witnessed profound transformations brought by artificial intelligence (AI). The integration of AI into HRM is evident in HR analytics, wherein statistical insights derived from personnel data are leveraged to inform HR and business decisions. However, the HR literature has lagged in providing theoretical insights and empirical evidence to address the growing integration of AI into HR analytics models. Scholars have critiqued that existing literature offers only ‘a glimpse into the variety of ways we can utilize these advanced methods to inform’ HR decisions. This research gap is critical and demands urgent attention, as it has significantly limited the impact and validity of AI-driven HR analytics, which rely on obsolete theories. The present study responds to the pressing demand arising from organizations’ aspirations to implement AI for competitive advantages, even in the absence of necessary theoretical analysis or accumulated knowledge in academia. This study adopts a relational view to understand and explore how responsible and effective HR analytics can benefit from analyzing workplace relationships, underpinned by the recognition that interpersonal dynamics profoundly influence organizational outcomes. Understanding these relationships offers a multifaceted perspective on employee behavior, performance, and overall workplace culture, which traditional HR metrics might overlook. I start with a review of the existing literature on HR analytics, HR digitalization, and relational HRM.
Based on this review, a comprehensive model of strategic relational HR analytics is conceptualized. This approach is defined as a data-driven, people-centric HR analytics model that emphasizes the analysis and evaluation of workplace relationships within and beyond organizational boundaries to make more ethical, responsible and effective personnel-related decisions. The model of strategic relational HR analytics is built on the premise that analyzing workplace relationships is essential for HR analytics, as it provides a comprehensive understanding of the human element within organizations. This analysis goes beyond traditional HR metrics to capture the nuances of employee interactions, which are critical for fostering a positive work environment, enhancing employee engagement, reducing turnover, improving communication, and promoting diversity and inclusion. I argue that only by capturing and evaluating relationships-related data can the model provide a complete picture of the organization, thereby offering more accurate and effective HR-related suggestions. For instance, diversity and inclusion initiatives benefit from the analysis of workplace relationships. Understanding how different demographic groups interact within the organization can highlight areas where inclusivity may be lacking. By examining the social networks and interactions among diverse groups, HR professionals can develop targeted strategies to promote inclusivity and ensure that all employees feel valued and included. As organizations increasingly recognize the value of their human capital, the insights gained from analyzing workplace relationships will be instrumental in driving strategic HR initiatives and achieving sustainable organizational success.
Author: Claus H. Jebsen (AS3 Norway; BI Norwegian Business School)
Background and Empirical Setting: As healthcare workers are faced with increasingly high quality & low-cost demands, higher complexity and less resources, the need for innovative, coordinated and collaborating practices requires leaders to lead within and beyond their defined agency, here understood as their “room for action” or “latitude”.
In this paper we study how leaders benefit from participating in a 6 module/20 days/10-month Executive Management Program. We look at how they develop their agency for the purpose of enabling partnership with collaborators within and outside the health sector. All participants are from the primary health care sector. The program curriculum is based on cutting edge research from the health sector (including sector relevant governance, law, economy and ethics), management literature and leadership training.
The pedagogical set-up in this program aims to make a practical impact on how the leaders lead, on the participants' home organization as well as on the health sector in general. Early engagement, role modeling, psychological safe climate, sharing experiences, discussing dilemmas and structured systemized reflexivity are examples of the pedagogical means. Boundary work, Relational Coordination, Psychological Safety, Communication Climate at Work, Reciprocity, Learning from Excellence and High Quality Relations are some of the theoretical frameworks presented in the program. Also, the participants are trained to foster improvement projects within their organizations. The applied method must be iterative, value realization oriented and executed in real life.
Data Collection: Each participant has submitted four reflection diaries regarding their co-creative practices. The student is evaluated on two exams; a 72hrs take- home exam focusing on their learning journey in connection to a given topic, as well as active use of relevant curriculum. In 2023 the topic was Tackling dilemmas, in 2024 it was “learning from failure”. The other exam is a 40-page report on their improvement project. Data are drawn from two different cohorts (2022-2023 and 2023 – 2024) providing us with submissions from 260 leaders, close to 780 reflection diaries, 260 home-exams and approximately. 130 improvement projects. Based on a qualitative research approach, the data has been analyzed using a combination of narrative, thematic and interpretative analytic approach. For this present paper, the focus has been on how the leaders increase their agency through involvement of “the others”, enabling multiple perspectives, shared goals and commitments.
Preliminary Findings: Our preliminary findings can be categorized into four groups: • Individual change and growth come from being vulnerable enough to learn, brave enough to try. • Relational change and growth come from being daring enough to confront, humble enough to listen. • Organizational change and growth come from inclusive, knowledge sharing practices enabling new routines, procedures, and practices. • Value realization innovates the sector.
Next Step: Prior to the RC Roundtable we will develop the paper and prepare a presentation that elaborates on how an EMP can enable leaders to see and act as part of the whole. I look forward to discussing these issues and further paper development together with the RC community.
Authors: Stephanie A. Hooker (HealthPartners Institute, Research and Evaluation Division), Julie A. Schmittdiel (Kaiser Permanente Northern California Division of Research), and Tainayah W. Thomas (Stanford University, Department of Epidemiology and Population Health)
Electronic health records (EHR) provide a large source of data on the health and well-being of populations. Observational research studies can use these data to answer important questions that would otherwise be difficult or costly to answer with other study designs, such as randomized controlled trials. Despite the impact of the findings of observational research studies using EHR data on stakeholders such as patients, caregivers, clinicians, health care leaders, and payors, there is little guidance on how to engage with these partners in EHR-driven research.
Our team recently outlined guidance for engaging these diverse partners in observational research to incorporate their voices into study design, conduct, and dissemination. The purpose of this presentation is to present our team’s “COORDINATE” principles for successful engagement of stakeholders in EHR-driven research, and to describe how our team incorporated these principles into an ongoing, PCORI-funded observational comparative effectiveness trial comparing four classes of diabetes medications (sulfonylurea, glucagon-like peptide-1 receptor-agonists, DPP4, and SGLT2 inhibitors) on cardiovascular outcomes in patients with type 2 diabetes. The parent study included EHR data from six health systems: Geisinger Health in Pennsylvania, HealthPartners in Minnesota and Wisconsin, Henry Ford Health in Michigan, and Kaiser Permanente in three regions: Northern and Southern California and Hawaii. The team recruited nineteen partners across the six systems, including seven patients, one caregiver, and 11 clinicians and health system leaders (including physicians, pharmacists, and a diabetes educator).
Engagement meetings were held biannually, for a total of 7 planned meetings over 3.5 years. Meeting topics included key questions related to exposure and outcome choices and definitions, reflections on potential confounders or factors associated with prescribing and use of medications, and considerations for future dissemination and impact of knowledge. Central themes from these meetings included the importance of medication cost and access/availability, health equity concerns, treatment burden, and informed choices on the multiple risks and benefits when considering which diabetes medication to prescribe or take.
Partners influenced the conduct of the study in a variety of ways, including: ranking the importance of several secondary outcomes to be considered in analyses, resulting in five additional planned manuscripts; signifying the best ways to define weight, kidney, and cardiovascular outcomes for maximal impact; encouraging investigators to reconsider analyses examining racial and ethnic differences in effectiveness of medications and further disaggregating Asian and Pacific Islander categories; providing feedback on the best ways to present results to improve broad understanding and dissemination; and suggesting future directions for this work.
These results indicate that engaging diverse partners in observational health research is feasible and can have a direct impact on the conduct, direction, and findings of these studies. We encourage researchers engaged in large observational studies to include voices from the people on which the data were collected, who understand how the data are typically used, and who may be interested in the outcomes of the work for clinical and system decision-making.
Author: Erin Blakeney (University of Washington)
Project Summary: We recruited (n=137) patients hospitalized with a diagnosis of advanced heart failure at a major academic center in Washington State to participate in a study to better understand their experiences with safety, communication, and bedside rounds on intensive and acute care units. Seven Relational Coordination (RC) questions were adapted to the context in consultation with RC Analytics and asked at the time of study enrollment and at ten-days post-discharge. Study recruitment was recently completed, and data cleaning and analysis are currently underway.
Context: Data collection occurred between August 2022 and June 2024. Study participants were recruited during hospitalization and were asked to complete questionnaires during enrollment and at ten- and thirty-days after hospital discharge. Additional data was collected via semi-structured hospital rounds observations, interviews, and electronic medical record review.
Methodology: RC questions were asked at the time of study enrollment and at 10-days post-discharge. At the time of study enrollment, participants were asked to complete the seven RC questions about the unit on which they were currently hospitalized. At ten-days post-discharge, participants were asked to complete the seven RC questions for units on which they stayed during hospitalization (intensive care and/or acute care unit). Study participants completed questionnaires either on paper or online via an email link to a REDCap survey. Participants received a thank you card and $5 cash or gift card upon completion of each survey. Preliminary RC results have been calculated as means and standard deviations at the individual question, domain (Communication or Relational), and Overall RC levels.
Findings: During the study period, 106 participants (77%) completed RC questions at the time of study enrollment and n=80 (58%) completed RC questions at ten days post-discharge. Preliminary results indicate that Overall RC was high (above a 4.0) at all time points and all settings (Enrollment = 4.44 (SD 0.6)), ICU Post-Discharge = 4.45 (SD 0.6), Acute Care Post-Discharge = 4.33 (SD 0.6). Of note however, at the question, domain, and Overall RC levels, scores were lower for those answering about acute care at ten-days Post-Discharge compared to RC questions at the time of Enrollment or about the ICU at ten-days Post-Discharge. The one exception to this was in response to the role question (framed in this study as “During this admission to the [unit], do people on your care team know about the role you want to take in your heart failure management?”). This question had the lowest score and the widest standard deviation for all time points and settings (Enrollment = 4.26 (SD 0.92)), ICU Post-Discharge = 4.27 (SD 0.96), Acute Care Post-Discharge = 4.24 (SD 0.85). Additional data analysis is underway to explore RC scores in relation to quantitative and qualitative patient- and family-reported safety and experience concerns, rounding model fidelity, and among demographically defined sub-groups (e.g. gender, race, education).
Authors: Stephen Schwab (University of Texas at San Antonio), Ingrid Nembhard (University of Pennsylvania), Robert Huckman (Harvard University), and Amelia Bond (Weill Cornell)
Background: Many hospitals staff their wards using a mix of permanent and temporary nurses. While permanent nurses give the hospital a predictable and consistent workforce, temporary nurses allow the hospital to flexibly increase staff during times of high demand without occurring the fixed costs of long-term employees. However, there are two reasons why temporary nurses might perform differently than permanent staff even if they have the same training and years of experience. First, temporary staff may be less familiar with the organization and the team they are joining. Second, temporary staff may exert less effort due to lower levels of organizational commitment. That is, they could have less “skin in the game” if the organization does not perform well. Conversely, though, nurses may be so committed to patient care that organizational commitment has little effect. In that case, any performance differences between temporary and permanent staff should be mediated by tenure within a nursing team. In this study, we quantify the productivity differences between temporary and permanent employees, and decompose any differences into turnover and organizational commitment mechanisms.
Context: We bring new evidence to this question through a novel data source: the Military Health System. Like its civilian counterparts, the Military Health System (MHS) staffs its hospitals using a mix of permanent civilian nurses and temporary contract nurses. The MHS has two unique features that provide an ideal testing ground for this question, though. First the military uses active-duty military nurses. The military moves these nurses between hospitals at least every 2-3 years. Furthermore, active-duty service members and permanent civilians are socialized into the organization from their first day of onboarding. Military creeds like “I will always place the mission first” and “Army Values” are explicitly instilled into these individuals but not into the temporary contract workers. These institutional details create an ideal testing ground for not only identifying the unbiased differences between temporary and permanent workers, but also unpacking any differences due to turnover compared to organizational commitment mechanisms.
Methods: We conduct this study by decomposing total productivity into three additive components: baseline productivity, organizational tenure driven productivity, and productivity gains due to team tenure. The baseline productivity is common to all employee types, with variation primarily driven by nurses’ formal training and total tenure as a nurse as well as any selection into temporary or permanent positions. Organizational tenure driven productivity is unique to military nurses and civilian permanent employees, as they are both long-term employees of the MHS despite the fact that active-duty military change work locations. Influencing factors of organizational tenure include but are not limited to aligned self and organizational identification and organizational commitment. The team tenure driven productivity is driven by accumulation of worksite-specific knowledge. Conditioning on the team tenure and individual-level experience and skills, we estimate differences between military and contract nurses in order to identify the impact of organizational tenure on productivity.
Authors: Shannon S Layton (University of Alabama at Birmingham School of Nursing), Shea Polancich (University of Alabama at Birmingham, School of Nursing), Patrick Pittman (University of Alabama at Birmingham Hospital, Interprofessional Skin Team), and Ross Vander Noot (University of Alabama at Birmingham, School of Medicine)
Background: An effective Learning Health System (LHS) culture is dependent on relational coordination (RC) which values learning, continuous improvement, systematic gathering of data and evidence, communication of data outcomes, the use of technology to inform decision making, promoting a positive continuous improvement feedback loop. LHSs integrate evidence with internal and external data to change both practice and processes thus producing a culture that yields high quality and safe patient care. RC is the key ingredient to successful implementation of new processes in complex matrix LHSs.
Purpose: The purpose of this study was to examine the role of RC in facilitating continuous, iterative improvement, redesigned workflow, standardized processes, and better resource utilization within a LHS. Existing relationships between structural and organizational characteristics were examined, focusing on those impacting HAPI adverse event outcomes.
Methods: We retrospectively examined longitudinal data from October 1, 2019-March 31, 2022, using a descriptive, observational design. Study variables were total number of all-stage hospital acquired pressure injury counts and average length of stay. An interprofessional skin team was organized, consisting of representatives across the health system and existing partnerships.
This dedicated 12 person wound care nursing team was created to treat all stage HAPIs. A data analytic tool was also created for effective management and outcome communication. Results: The relationship between average length of stay and HAPI was evaluated using correlation analysis. HAPI rates per 1,000 patient days decreased from 2.3 to 1.3 across pandemic affected fiscal year (FY) 20 and FY 21. A strong negative correlation was found to be statistically significant (r=-.524, p=.003). Estimated AHRQ cost savings from reduced HAPI events totaled $4,786,980 annually.
Conclusion: Using RC, our leadership and workforce produced a LHS transformational outcome through reduction of HAPI. RC was present in facilitating effective use of data to drive iterative processes, increase workforce and organizational commitment to continuous learning and safe patient outcomes and quality care.
Authors: Whitney K. Onasch (Kansas University Medical Center), Hebatallah Naim Ali (Brandeis University), Carolyn F. Caine (Kansas University Medical Center), Zseraldina Ferenczi (Kansas University Medical Center), Rashna Madan (Kansas University Medical Center), Wei Zhang (Kansas University Medical Center), Andrew K. Godwin (Kansas University Medical Center), Jody Hoffer Gittell (Brandeis University), Shellie D. Ellis (Kansas University Medical Center)
Background: Precision oncology is a promising direction for cancer care and relies on complex guidelines around genomic testing. Reflex testing, in which pathologists initiate genomic test ordering, is an evidence-based strategy for improving concordance with guidelines and decreasing time from diagnosis to treatment decision-making. For some health systems, reflex testing requires shifting primary responsibility for genomic test ordering from oncology to pathology. This change necessitates effective inter-team communication.
Methods: We conducted a sequential, mixed-methods analysis of a survey of oncology and pathology teams at a not-for-profit, independent hospital authority. Participants completed the 7-item Relational Coordination Index and answered questions about communication and test ordering. The survey was administered at two time points three months apart to establish a baseline. We conducted a t-test to determine the validity of aggregating the two baseline waves of the survey; we found no statistically significant difference in relational coordination measures across the two time points. Subsequent analyses included the development of logit models to assess the impact of the overall Relational Coordination Index and its 7 dimensions on recognition of pathologists’ role in genomic test ordering. We conducted sensitivity analyses to identify variations in outcomes among subgroups.
Findings: The aggregated dataset reflects a 78.3 percent response rate (301 responses from 384 participants). Participants were asked how frequently they order genomic tests. We find that pathologists are most likely to report a high volume of test orders, i.e., ordering genomic tests more than 20-times per month (19.35 percent compared to 6.92 percent for medical oncology and 0 for radiation oncology). However, just 31 percent of participants regard pathologists as having a primary role in ordering genomic testing. This finding suggests some pathologists see genomic test ordering as part of diagnosis and conduct reflex testing, but capacity is minimal at this point. Our models suggest a 1-point increase in relational coordination score doubled the odds that participants recognize pathology as having primary responsibility for genomic test ordering. Two dimensions of relational coordination—problem-solving communication and shared knowledge—boosted the odds that participants recognize a primary role for pathology. The Relational Coordination Index was associated with recognition of pathologists' role in genomic test ordering, even after controlling for (1) site type, community or academic, and (2) cancer service line. Among pathologists, a one-point increase in the Relational Coordination Index results in a five-fold increase in the odds of a pathologist ordering at least one genomic test per month, suggesting that higher levels of relational coordination increase the likelihood that pathologists will order genomic testing.
Conclusions: Findings reinforce the value of interventions to improve relational coordination before shifting more responsibility for genomic test ordering to pathologists. These results point to the value of building shared knowledge and problem-solving communication for effective reflex testing implementation.
Authors: Hilary Nichols (Oregon Health & Science University RELATE Lab), Brian Park (Oregon Health & Science University RELATE Lab), Leah Gordon (Oregon Health & Science University RELATE Lab), and Matthew Lewis, (Oregon Health & Science University RELATE Lab)
Advancing health equity is an increasing priority for the U.S. healthcare system, with significant resources being devoted to addressing the social factors influencing health. However, efforts to address social needs within healthcare may not only be inadequate, but may also inadvertently exacerbate health inequities. For example, social needs screeners are known to favor individuals who can more readily access healthcare, and services may preferentially meet the needs of dominant cultures (e.g., emergency food boxes that are not culturally responsive). Moreover, these efforts do not address the root cause of health inequities: socially-constructed power imbalances that disproportionately impact systemically harmed communities (e.g., Black, Indigenous, and People of Color [BIPOC]; LGBTQ+ communities).
Relational Community Organizing (RCO) holds promise to support health systems to advance health equity by building inclusive and resilient communities. RCO is an approach to social change in which community members identify the issues most impacting them, build relationships with one another, then act on those issues together. Through connecting over shared values and social pressures, community members build power together to achieve socio-political change, develop long-term relationships, and sustain collective action.
RCO employs time-tested strategies and tactics - including campaigns, advocacy, direct action - to improve social conditions and improve health of oppressed peoples. Launched in 2015, Health Equity And Leadership (HEAL) is a clinic-based RCO initiative at the Oregon Health & Science University’s Richmond Clinic (a community health center in Portland, Oregon). HEAL locates the clinic as a geographic base where community members share their lived expertise through identifying social pressures most impacting them and their loved ones. They engage in power building through learning key skills in community organizing, and practice solidarity by building relationships together - of patients, community members, healthcare workers - to address priority structural factors of health and equity.
With a Health Equity Community Organizer on staff, HEAL conducts listening sessions, leadership trainings, and builds local campaigns to address issues most impacting community members, including advocating for health system changes that align with community priorities. HEAL’s emphasis on building multi-sectoral relationships and centering the leadership of systematically harmed leaders has led to several impacts.
HEAL’s policy impacts include: 1) a Portland bill that led to an additional $67 million for affordable housing, 2) an Oregon bill mandating non-English languages be translated on prescription drug labels (the most inclusive bill of its type in the U.S.). HEAL also launched a social connection program during the COVID-19 pandemic, with over 100 isolated community members receiving longitudinal connection phone calls for nearly 2 years. Current efforts involve a leadership team with lived expertise of justice involvement, who are leading the creation of a healing center for justice-involved individuals reentering the community. Qualitative evaluations demonstrate participants feel listened to by people with power, increased confidence in defending one’s rights, and increased social networks to collaborate with others. HEAL offers a model for how a health system can implement a relational community organizing infrastructure, with a community health center as a hub to develop meaningful change campaigns.
Author: Lorinda Visnick (University of Massachusetts Boston)
Summary: This session will address cross sector coordination and boundary spanner roles. I will introduce the concept of using housing as a services hub as an approach to move individuals out of poverty. We begin with an overview of the approach, including an explanation of how one boundary-spanning individual and their team are working to orchestrate dozens of social service providers that each try to help those in poverty.
Context: America has an expanding housing crisis. Part of the problem is a housing shortage. Like any supply and demand issue, when demand rises and there is not ample supply, prices rise. Consequently, millions of low- and moderate-income people are priced out of the housing market; they are either housing burdened or unhoused. Wealth inequality has increased multi-fold since the 1980’s. Quite literally, the rich are getting richer and the poor are getting poorer. Consequently, there are more people experiencing poverty. It is within this set of circumstances that we find a plethora of social service providers working to combat the suffering of those in poverty. In addition to the social service providers, there are organizations working to increase housing stock, especially affordable housing.
Research: In Beverly, MA there is a community development corporation (CDC) that is providing more than just housing. This organization, and specifically the Executive Director, is providing both deeply affordable housing and a set of comprehensive wraparound services for residents of the housing complex. I begin a PhD program in Public Policy in September, 2024, with a focus on housing. It is my intention to formally study this family-based housing complex and the approach being taken there. My expectation is to use an RC lens to measure this CDC along with measuring the outcomes of residents in the complex. I expect my research questions to include: - Do adult residents change income brackets - Do child residents improve academic outcomes (attendance, graduation rates, standardized test scores) - How do residents identify; does that self-identify change over time after taking part in some number of the services offered on site
Expected Findings/Takeaways: I believe using housing as a services hub is worthy of formal study; however, I believe there’s more to examine. Specifically, other similar organizations are providing service-based housing. In addition to resident outcomes, I expect to measure the relational coordination of the organizations (and their leaders) that offer service-based housing to then compare and contrast resident outcomes relative to the RC scores.
Authors: Chris Rubeo (School of Public Health, UC Los Angeles), Melie Ekunno (School of Public Health, UC Berkeley), Amanda L. Brewster, (School of Public Health, UC Berkeley), and Emmeline Chuang (School of Social Welfare, UC Berkeley)
Background: People experiencing homelessness have high rates of co-occurring physical health, mental health, and substance use disorders compared to housed people. The complexity of seeking services from multiple organizations in separate care systems is a known barrier to care. Coordinating social and medical care can improve access to care, housing retention, and health outcomes for chronically homeless individuals. However, coordinating care across sectors is challenging due to the need to align operations and services across organizations that may have very different priorities, regulations, funding, staffing, and capacity. Little is known about how organizations working in these sectors can effectively coordinate care for this population.
Relational coordination theory proposes that frequent, timely, accurate, problem-solving communication is essential for effective care coordination, and that this communication is facilitated when people share goals, knowledge, and mutual respect. Informed by relational coordination theory, this study examines organizational structures and relational practices that enable stakeholders from the health and housing sectors to effectively coordinate their work.
Methods: Stratified purposeful sampling was used to select organizations identified as leaders in effectively coordinating medical and social care for unhoused people in Los Angeles County. Between October 2022 and September 2023 we conducted 54 interviews with staff at homeless services agencies (n=19), healthcare provider organizations (n=17), local government agencies (n=12), and managed care plans (n=6). We also conducted six site visits to observe coordination in the field. Interview transcripts and observation notes were coded and analyzed using a primarily deductive approach, with codes corresponding to structures identified as facilitating relational coordination (e.g. boundary spanner roles, shared space, shared information systems).
Results: Medical and homeless services providers recognized the importance of coordinated care and expressed a belief that it made both medical and housing support services more accessible and effective. Study participants from both sectors described using several approaches to coordinate care that aligned with organizational structures predicted by relational coordination theory. The most frequently identified structures included shared space (co-locating services, jointly staffing teams), shared meeting and huddles (case conferencing), and boundary spanner roles (liaisons). Due to a lack of shared information systems, participants reported relying heavily on informal communication to coordinate care. Finally, participants emphasized the importance of relational leadership at both the administrative and frontline levels.
Conclusions: Few organizations have the services and capabilities necessary to meet the full range of care needs of people experiencing homelessness. We found that medical and social care providers were highly motivated to coordinate care and they frequently leveraged organizational structures such as co-located services, jointly staffed teams, and case conferences to bring care providers from different sectors together into the same place or onto the same team to improve coordination. Further, we found that effective coordination depended on strong interpersonal relationships among frontline providers, and that relationships and structures at the individual and organizational levels interact and are mutually reinforcing. These findings suggest that organizations seeking to coordinate care should couple investment in infrastructure with attention to the experience of front-line providers.
Author: Cady Landa (School of Social Work, University of Illinois Urbana-Champaign)
Overview: This presentation will share the research methods and key findings of mixed methods research examining the access of young children of immigrants to public education entitlements in one state. It will focus on the use of relational coordination theory to understand barriers that prevent school staff from meeting needs of individual students. It will also cover how the relational bureaucracy framework could be used as a model for increasing school responsiveness to individual students, aiding in the integration of immigrant parents and their children, and engaging the school community in a process of adapting school practice to changes in the population served.
Methods: The case study used relational coordination theory as a lens for examining the impact of school organizational structure on the response of school staff to the needs of the 11 students. It examined the extent to which school organizational structures supported and thwarted within-staff and staff-parent coordination in ways that impacted the timeliness and quality of the school’s response to these students.
Findings: A multivariate analysis of Massachusetts education data found that children of immigrants in grades K-5 are significantly less likely than children of U.S.-born parents to participate in special education. It also found that among children who do participate in special education, children of immigrants are more likely to be in substantially separate settings and less likely to be in inclusive settings than are children of U.S.-born parents. A companion case study of a Massachusetts elementary school sought to understand these results by examining how school organizational structure as well as public policies affecting immigrant parents and schools affected the capacity of the school staff to respond to the needs of 11 children of immigrants in grades pre-K through 5.
Implications: Public schools, developed in the early 20th century, are predominantly bureaucratic in structure, featuring a focus on large groups rather than individual students, solo teacher practice, and vertically siloed departmental staff. This study demonstrates the importance of schools having sufficient resources to move towards a more relational structure that supports within-staff and staff-parent coordination on behalf of individual students in the pre-K and early grades. It also demonstrates the importance of providing language access and systems knowledge to immigrant parents so that they may effectively coordinate with school staff and navigate schools and other systems on behalf of their children.
Authors: Katherine Bartz (UC San Francisco), Kelly Brandon (Zuckerberg San Francisco General Hospital), Mara Fox (Zuckerberg San Francisco General Hospital), Christy Boscardin (UC San Francisco), and Maytinee Lilaonitkul (UC San Francisco)
Introduction: Labor and Delivery (L&D) units are vulnerable to breakdowns in teamwork due to complex dynamics between different disciplines.1 This can lead to silo mentality, power differentials and conflict. Interprofessional simulation-based team training (ISBTT) is a vital L&D teamwork improvement tool. ISBTT debriefing often focuses on correct execution of hierarchical protocols and rarely addresses team behavior interdependency.
Relational Coordination (RC) theory quantifies social processes and human interactions.4 The seven RC domains include three relational aspects (shared knowledge, shared goals, mutual respect) and four communication aspects (frequency, accuracy, timeliness, problem solving). RC has been used to improve interdisciplinary teamwork, but literature on L&D unit RC-informed ISBTT is lacking. Hypothesis: L&D unit team dynamics can be evaluated through RC-informed ISBTT.
Methods: IRB exemption was obtained (#22-36662 UCSF). A baseline validated RC survey was distributed to ZSFG L&D team members. Data were analyzed using RC SurveyTM. Using these data and the seven RC domains, a standardized ISBTT debrief guide was created. ISBTTs are held monthly on the L&D unit. Sessions include two 15-min cases on leading causes of maternal mortality reported by the CMQCC, followed by 30-min debriefs. Debrief audio recordings are thematically coded to the seven RC domains via DedooseTM.
Results: The baseline RC survey response rate was 27% (68/255). Results showed an RC index of 3.76/5 indicating moderate RC among all L&D team members. Seven ISBTT sessions were held from Aug 2023-Mar 2024 with 84 nursing, midwifery, OB and anesthesia staff and trainees. Participants’ evaluations on debrief effectiveness in addressing team dynamics and communication showed a mean rating of 4.74/5 (SD 0.81, Likert scale). Interim data analysis of 216 min of debrief recordings revealed 486 thematically coded excerpt. RC domains with the highest prevalence were shared knowledge (26%), mutual respect (16%), timely communication (12%) and accurate communication (11%). RC domains with less prevalence were shared goals (9%), problem solving communication (6%) and frequent communication (1%). Other thematic codes occurred with 19% frequency.
Discussion: Interim analysis suggests RC theory can be effectively applied to L&D ISBTT. Shared knowledge (perspective taking and understanding team roles) was most commonly addressed (26%). Frequent communication was least addressed (2%), possibly due to 15-min case time constraints. These findings aid in assessing team dynamics and may promote culture change in teamwork and communication. Conclusion: L&D unit team dynamics can be evaluated through RC-informed ISBTT. This allows the quantification of complex team interactions and may promote culture change.
Authors: Erin Collins (Concord Hospital Health System) and Laura Montville (Concord Hospital Health System)
Context. Concord Hospital-Concord is the core hospital within the growing Concord Hospital Health System in central NH. The System places high priority on both people and efficiency. Current financial headwinds raise challenges for health care organizations across the country necessitating a need to balance productivity and education, training and development of the workforce. The System will embark on a transition to a centrally coordinated nursing education model to target a standardized, integrated education approach with a focus on improving the relational dependencies of a newly created centralized nurse educator team.
Methods. In Summer 2024, the Senior Nurse Executive proposed the use of relational coordination principles and methods to build a synergistic, high-relational educator team who would drive improved efficiencies and productivity of the nursing orientation and onboarding process. Ultimately using a relational efficiency and process improvement approach as an alternative to workforce reduction to meet productivity targets. This work is actively in progress and the System will analyze the current state with the educator team using tools - relational mapping analysis, RC survey and organizational structures assessment. The System will then propose interventions to strengthen central education structures, relational coordination and desired performance outcomes.
Findings. After the initial assessment, significant variation in the routine nursing orientation process specific to duration, content and tracking was identified. Additionally, the nurse educators have been used to backfill open shifts when there are shortages and are pulled away from their primary education duties. These conditions resulting in nurse educator stress, process inefficiencies, and dis-satisfaction of new hires has created a call to action. The goal is to optimize an effective central education team to deliver consistent, standard and efficient onboarding training, which will yield a significant reduction in worked hours, improving productivity and reducing costs while improving the nurse experience and retention.
Next Steps. Over the next few months, the System will prioritize the work with a primary focus on building a centralized nurse educator team using the relational coordination principles and methods. They will then engage the central education team to re-design the nursing education and orientation process with shared goals, mutual respect and improved communication. Lastly, the System will evaluate the relationship of the newly centralized education team to the nurse managers of the patient care units to ensure optimal partnership in the support and education of nurses in the System.
Authors: Deborah Blackman (UNSW Canberra), Fiona Buick (UNSW Canberra), Jean Hartley (Open University), and Nicky Miller (Open University)
Collaborative research efforts between academia and public sector organisations have long been recognized as potentially beneficial (Mullin, 2021). Academic-practitioner research partnerships are a particular form of inter-organisational, cross-sectoral collaboration designed to create new knowledge supporting impactful public outcomes. However, despite enthusiasm for collaborative arrangements, they frequently fail with a large body of literature trying to understand the phenomenon (Bender, 2022). We suggest that the focus on boundary spanning to solve partnership challenges has failed to enable system change and we offer a reconceptualized system of partnerships.
We posit adopting a relational orientation is core to this reconceptualization. As Bradbury and Lichtenstein (2000, p.551) argue, “Taking a relational orientation suggests that the real work of the human organization occurs within the space of interaction between its members. Thus the theorist must account for the relationships among, rather than the individual properties of, organizational members” According to this perspective the stories about the individuals do not exist outside of the relationships with other people. In other words, relationality suggests that the nature of something is determined by its relationships with other things, rather than only by its inherent qualities or properties. We suggest that thinking about relationality in this way may explain why boundary spanning creates the counterintuitive behaviour of entrenching, rather than bridging within a system. The emphasis on translating existing languages and adapting and changing existing processes at the edge of these systems, triggers feedback loops that either maintain steady state or even makes things worse.
This paper draws on evidence from two case studies: Strengthening Performance Frameworks (Australia) and the Centre for Policing Research and Learning (UK). Each case is a successful programme of research undertaken within an academic-practitioner partnership over an extended period. The case studies used in this paper are both retrospective, based on systematic reflection by, and dialogue between, a range of academics and practitioners.
We use the case data to propose an alternative conceptualisation: that of the academic-practitioner partnership as creating and sustaining a new, open and purposeful system for at least the duration of the project. This system is co-designed specifically for the purpose of partnering and co-producing knowledge through which novel outcomes may emerge that serve the public good. At its core is a relational orientation, which enables members to find ways of working with, rather than against, the differences in values, goals and interests among the partners. Perhaps counter-intuitively, we propose that this new, single system perspective offers different ways to intervene that enable better and more sustainable outcomes for inter-organisational partnerships.
Author: Lester F. Bussey (Nuvance Health)
Background: In the late 20th century, global healthcare faced a significant crisis as described by reckoning. Frenk et al. (2010). The evidence suggested a disconnect between prioritizing patient and population needs and practitioner competencies. By 2016, the American Council of Graduate Medical Education (ACGME) Milestones were universally implemented in U.S. Obstetrics and Gynecology (Ob/Gyn) residency programs. Yet, despite providing a rigorous framework for assessment, realization remains a challenge. Inter-rater variability is high, and faculty commonly note they are complex to use.
Purpose: The author endeavors to assess the quality of relationships and collaboration among nurses, faculty members and Ob/Gyn residents using the RC Survey 2.0. Theoretically, the Clinical Learning Environment (CLE) of an Ob/Gyn resident can be visualized as a nested ecosystem and community of practice in which the sponsoring institution (mesosystem) serves as a barrier or facilitator of IPECP (Interprofessional Education and Collaborative Practice) and the relationship between the trainee (microsystem) and the ACGME (macrosystem). The research introduces and utilizes the novel Relational Coordination Action Framework for Health Professions Education and Practice (RCAF-HPEP), which fuses the IPECP Framework for Patient-Centered Care with the RC framework for performance improvement through the Quintuple Aim. This framework has not been previously discussed in the literature. The research seeks to identify opportunities for improvement and contribute to the overall goal of enhancing IPECP.
Research Questions: 1. Does physician experience level (grouped by Faculty, PGY I, PGY II, PGY III and PGY IV) have a statistically significant impact on physician-nurse relational coordination (RC)? H0: There is no statistically significant difference in the impact of physician experience level on physician-nurse RC. 2. What is the relationship between PGY IV IC/IPECP milestone data and PGY IV RC data? H0: There is no statistically significant relationship between PGY IV milestone and RC data. 3. In a nested ecosystem and community of practice, what do stakeholders perceive as the barriers and facilitators of IPCP?
Study Design: Our goal is accomplished by building on the work of WHO and Dr. Jody Hoffer Gittell, fusing the IPECP Framework for Patient-Centered Care with the RC framework for performance improvement through the Quintuple Aim. RC is a mutually reinforcing process of communicating and relating for task integration. Researchers distribute the RC Survey 2.0 monthly to nurses, faculty members, and PGY I – PGY IV residents assigned to the labor floor. The one-way ANOVA determines if physician experience impacts physician-nurse RC. The Spearman’s Rank Correlation analyzes the relationship between PGY IV RC-Survey and Milestone data. Cronbach’s alpha and Exploratory Factor Analysis enhance validity. Semi-structured focus groups and deductive analysis offers insight to how institutional and professional culture impact IPECP through RC.
Conclusion: By enabling more comprehensive analysis and intervention design, this study aims to identify improvement opportunities and enhance interprofessional education and collaborative practice in Ob/Gyn residency programs through the novel RCAF-HPEP framework. By examining RC among healthcare professionals and its relationship to educational milestones, the research offers a seamless view from education to practice. This integrated approach promises lasting improvements in healthcare delivery.
Author: Darren McLean (Griffith University)
The Relational Model of Organizational Change (RMOC) has been used in hospitals to facilitate practice improvement. However, this application of the RMOC is believed to be challenged by invisible power dynamics. Yet, the nature of these power dynamics and the mechanisms through which they exert their influence is not fully understood, creating a knowledge gap that if addressed would help support those wanting to use the RMOC within hospitals.
In our study, we applied Institutional Ethnography (IE) to examine institutionalized power dynamics (ruling relations) surrounding the implementation of the QPH RC Program: a program that used the RMOC to facilitate practice improvement in a public tertiary hospital in Australia. Ruling relations are dominating social processes (e.g., ubiquitous discourses) that originate outside of organizations to regulate and organize people’s work within organizations. They exert their effect via textual mediation, whereby texts act as a go-between amongst the people participating in social processes and the ruling relations shaping those processes.
Methods: Consistent with IE, we started from a problematic whereby the first author and colleagues were concerned that the intrinsic relational work within the QPH RC Program was devalued. Hence, we interviewed program implementors, program participants, and organizational leaders to understand their challenges and their work and identify texts used to regulate and organize this work. The texts were then analyzed as ‘texts-in-action’—examining how people used them. We then searched within the texts for embedded representations of discourses (i.e., speech genres), leading us to reveal ruling relations and map connections between those ruling relations, the texts, and the work of implementing the QPH RC Program.
Findings: Improving team communication and relationships within the hospital (relational work) was perceived to be disproportionately devalued against other initiatives that focused predominantly on improving financial objectives. In practice, a Service Agreement (SA) between government bureaucrats and hospital leaders functioned as a chief regulatory text, specifying the priorities for the organization, and used by organizational leaders to direct improvement initiatives in the hospital. Relatedly, project management documents were used to align the focus of the QPH RC Program with the priorities in the SA, while RC texts (e.g., books about the RMOC) were used to inform the implementation process. Within the SA were representations of economic rationalism—a ubiquitous discourse, a ruling relation, that prioritizes financial objectives in public sector organizations. Ultimately, a textually mediated connection was shown between the SA and the work practices targeted for improvement, with priority afforded to those addressing financial objectives over objectives to improve team communication and relationships, the essential work of the QPH RC Program.
Implications: These findings have important implications relative to seeing the whole together through relationships and networks. Our findings suggest that those interested in using the RMOC to address issues of equitable healthcare must pay attention to institutionalized power dynamics (i.e., dominating discourses) that influence what gets prioritized for improvement within hospitals. Further research is recommended to understand more about how challenging power dynamics can be addressed through the RMOC.
Author: Claus H. Jebsen (AS3 Norway; BI Norwegian Business School)
Context: In Norway primary health care is governed by the municipalities and the specialist health care is run by the state through the hospitals. Despite collaboration reforms, “patient flow” initiatives, collaboration between the two sectors remains challenging. As a strategic initiative the former Health Minister sponsored a 6 module/20 days/10 months top management program for 22 leaders from each health care sector. Main purpose of this 30 ECST Execute Management Program (EMP) is to increase and support innovative collaboration between the two sectors, driving sustainable solutions to real life problems and ensuring that the patient experiences a seamless journey.
The curriculum covers research from all major topics relevant for top managers, such as governance, digitalization, innovation, top management groups, health economy etc. The modules support two paths which run throughout the program: personal leadership development and improvement project. While personal leadership development increases awareness, skills and models for individual leadership practice, will the improvement project through an iterative approach seek and implement possible solutions to defined real life problems. Each improvement project is conducted in groups of 4, equally represented from either health care sector. This paper delves into how Relational Coordination Theory might enable a profound shift in how top managers understand and lead coordination and collaboration within and across entities.
Methods: Data are sampled from two cohorts, class of 2023 and 2024, with a total of 84 top-managers. We draw data from observations from class as well as from 30 hrs of facilitating a smaller “learning group." Data are also collected from two different exams: 84 individual 72 hour take-home exams focusing on their learning journey considering a given topic, as well as active use of relevant curriculum, and 22 40-page improvement project reports. Not all participants have decided to report their use of Relational Coordination Theory. For those who have, data are analyzed using a narrative and thematic approach. In particular we seek to learn what triggered the participants to use a RC approach, what were the gains and how did it enable a desired change.
Preliminary Findings: We are early in the analysis as the final exams were recently submitted. However, so far three topics call for further attention. 1) RC mapping exposes existing ignorance of the other, meaning each actor knows little of the other - and all require that the others “should” know more. This call for humble, but straight, sharing of information. 2) RC framework ignites curiosity and exposes willingness to know more of “the others”. This fosters perspective taking and making as part of finding sustainable solutions. 3) It reminds the participants that each actor is part of a whole and that it is necessary to sustain the whole as well as its parts. This awareness shapes their leadership practices Next Step: This is an ongoing work and the paper will be developed towards Roundtable. I would appreciate the opportunity to present and discuss with the RC community how RCT can serve as a game changer for top managers in complex organizations.
Authors: Yujin Lee (University of Massachusetts Boston), Anne Douglass (University of Massachusetts Boston), and Kyungmin Kim (Seoul National University)
Study Summary: Effective leadership within early care and education (ECE) programs is essential for enhancing work environments, classroom quality, and children’s outcomes. However, there is little empirical research on how leadership contributes to better outcomes for early educators and for program quality, and the mechanisms through which leadership impacts these outcomes. This research aims to assess the extent to which instructional leadership practices implemented by program leaders (e.g., facilitating data dialogues to guide curriculum adjustments and teaching practices, and hosting regular planning sessions where teachers can share ideas and strategies) are associated with teacher commitment to their workplaces and active engagement in collaborative job-embedded professional learning (JEPL). Examples of collaborative JEPL include participating in peer observations to offer feedback, jointly analyzing child data, and co-developing instructional materials or classroom activities.
Central to our investigation is the concept of relational coordination, which involves shared goals, knowledge, and mutual respect and high quality communication within and across roles to achieve high-quality performance. We hypothesize that higher levels of leadership practice implementation are associated with stronger teacher commitment and more active participation in collaborative JEPL. We also hypothesize that relational coordination serves as a significant mediating pathway, channeling the effects of leadership practices into positive outcomes for teachers.
Study Context: Since 2021, Early Education Leaders has implemented the Essential Leadership Model (ELM) in MA ECE centers to improve instructional quality. To date, the ELM initiative has successfully recruited four cohorts, which included 75 leaders from 32 programs across the state. A recent ELM evaluation study has found that despite the challenges of the COVID-19 pandemic, the initiative has maintained high retention rates. Also, engaged leaders were found to actively implement instructional leadership practices within their ECE programs. This study aims to further explore the specific benefits and impacts of the ELM by promoting instructional leadership practices among program leaders, specifically in terms of enhancing relational coordination, teacher commitment, and collaborative JEPL.
Study Methods: Our study drew data from the first two cohorts of the ELM initiative. Forty leaders from 17 center-based ECE programs in Massachusetts participated in the initiative, engaging in comprehensive training, coaching, and peer learning communities to enhance the implementation of instructional leadership practices. At the conclusion of a 2-year initiative, ELM coaches reported the implementation of instructional leadership practices at the program level. Teachers (N = 208; from 17 center-based ECE programs) rated dimensions of relational coordination at their program. They also reported their commitment to their workplace and their engagement in collaborative JEPL. We will use path analysis to understand both direct and mediated pathways through which leadership practices influence teacher outcomes.
Key Takeaways: Our study findings can highlight the essential role of effective ECE leadership in fostering a supportive and high-performing work environment for early educators. Additionally, this study aims to illustrate how relational coordination within ECE programs can serve as a powerful mechanism for program improvement. Thus, our study can showcase the benefits of integrating relational coordination theory into ECE professional development efforts to promote educator outcomes.
Authors: Hun Lee (The Ohio State University), Jooyoung Kim (Deakin University), Hanho Lee (The Ohio State University), and Maria Triana (Vanderbilt University)
Grounded in the symbolic and substantive frameworks of senior leadership's impact, our study illuminates the cascading influence of female representation in Top Management Teams (TMTs) on fostering effective coordination among gender-diverse employees, leading to improved group performance.
Our empirical investigation encompasses panel data (Study 1: 1,017 observations across 306 firms over eight years) and two group-level surveys (Study 2: 93 leaders and 391 members; Study 3: 47 leaders and 149 members), all within the context of South Korea.
Consistently across our studies, we find that the positive indirect effect of employee gender diversity on group performance, mediated by relational coordination, is significantly amplified by increased female representation in TMTs. Notably, Study 3 reveals that it is TMTs’ substantive influence (e.g., diversity-supportive practices and initiatives), rather than their symbolic influence (e.g., signaling equal opportunity for career advancement), that underpin the observed benefits of female representation in TMTs. Our research highlights the pressing importance of advancing the representation of women in top leadership positions.
Authors: Laura Rees (Oregon State University), Tony Dejun Kong (University of Colorado, Boulder), Liuba Y. Belkin (Lehigh University)
With the rapid increase in technology-mediated interactions (Lumineau et al., 2023), people often find themselves in zero-acquaintance interactions. In traditional (face-to-face) business encounters at zero acquaintance, individuals typically spend some time chatting before diving into the task at hand. Such chats, also known as small talk (i.e., brief, superficial communication unrelated to the task at hand; Malinowski, 2000/1923), serve important relational functions (Molinsky, 2013) and help build trust (Lu et al., 2017). Building swift trust—rapidly evolving trust that is limited in time and scope (Meyerson et al., 1996)—is particularly important in virtual interactions at zero acquaintance, which involve high uncertainty. In such contexts, emotional expressions during small talk can aid swift trust building, as emotions communicate social information about the expresser’s goals, motivations, and behavioral intentions (Keltner & Haidt, 1999; Rees et al., 2020), quickly shaping initial impressions of others (e.g., Belkin & Rothman, 2017). Moreover, unlike traditional environments, the asynchronous, text-only virtual context in particular lacks other cues available to interaction partners and thus increases the salience of emotional expressions (Derks et al., 2008).
Ironically, the nature and quick pace of the virtual context adds pressure to limit or eliminate small talk, thereby impeding trust and relationship building in an already difficult-to-navigate environment (Thompson, 2023). We challenge this practice and propose that emotional information conveyed in virtual small talk prior to discussing the task at hand can provide an easy and useful means of swift trust building among strangers, with different emotions fostering swift trust through different mechanisms. Prior work has shown that “schmoozing” before a negotiation can be beneficial for building rapport and trust (Morris et al., 2002). Both rapport—feelings of being “in sync” or on the same wavelength (Drolet & Morris, 2000)—and identification—interpersonal interconnectedness and closeness (Aron et al., 1992)—are related to the perceived connection between individuals. Beyond the interpersonal connection, expressed emotions that deviate from social norms can also convey authenticity (Pillemer, 2024), as such emotions are more diagnostic of the expresser’s true psychological state or character. Therefore, we propose three distinct mechanisms that can facilitate swift trust in virtual environments in response to an emotion expressed during small talk: perceived partner authenticity, felt rapport, and identification with the partner. We consider both positive and negative emotions of varying valence and activation that represent the five groups of emotions proposed by Baas and colleagues (2008)—happiness, relief, anger, worry, and disappointment—to comprise a robust comparison set to a neutral (no emotion) state expressed during small talk.
Across studies (N = 1,444; both with U.S. Prolific Academic workers and U.S. university students), we found consistent evidence that, compared to a neutral (non-emotional) partner, participants developed stronger trust toward those who expressed happiness, relief, or anger during small talk, but through different mechanisms. By showing the three different pathways—perceived partner authenticity, rapport, and identification with the partner—our research sheds novel light on swift trust building and relational coordination in virtual environments.
Authors: Alexis Amano (VA Greater Los Angeles; UC Los Angeles Fielding School of Public Health), Seppo Rinne (Bedford VA Medical Center; Dartmouth Geisel School of Medicine), and Julian Brunner (VA Greater Los Angeles)
Background and Aims: Health care system transitions from one electronic health record (EHR) to another are becoming more frequent but can be disruptive to care delivery. Because shared information systems, including EHR documentation and in-basket messages, are central to relational coordination in health care, an understanding of EHR transitions’ impact on interpersonal relationships and communication is needed. In this analysis, we investigate health care workers’ perspectives of an EHR transition’s impacts on the workflow, norms, and quality of communication within teams.
Methods: Longitudinal, semi-structured interviews were conducted with clinicians, nurses, support staff, and clinical administrators (n=27) at a Veterans’ Health Administration (VHA) facility transitioning from a homegrown EHR to a commercial system 2-months pre-go-live, 2 months post-go-live, and 10 months post-go-live to assess general EHR transition experiences. Data were analyzed using a combined inductive and deductive approach.
Results: Analyses identified four key changes in interprofessional roles, norms, and expectations reported by participants: (1) The new system, which was optimized for hospitals or clinics that refer to outside pharmacies, diminished opportunities for chart-based bidirectional communication between clinicians and pharmacists, impeding the VA’s close integration of pharmacy and clinic-based care; (2) the new system enabled users to send messages in multiple ways; however, these changes were implemented without a mechanism to establish corresponding norms and standards, resulting in ambiguous and inefficient communication; (3) the new EHR introduced the ability for messages to be routed to and managed by groups – a change that some respondents welcomed and described as supportive of collaborative message management, but many found challenging to adapt to; and (4) while adapting to these changes, teams turned to workarounds outside of the EHR, including email and workplace instant messaging, to communicate.
Conclusions: A health care system’s EHR shapes the way in which health care teams communicate and relate to one another. Thus, EHR changes that are conducive to relational coordination are needed. Prior research has identified a positive association between shared information systems and relational coordination. Our findings contribute to a growing body of research that adds nuance to this association. We highlight the importance of an EHR that is designed to support communication and increase the visibility of workflows. Additionally, our findings build on a limited literature base about the implementation of information systems. We identified that health care systems can support users during EHR transitions by preparing teams for altered communication workflows and by proactively communicating expectations and establishing norms for how new communication functionality will be used. Doing so will support ongoing relational coordination during transitions and reduce reliance on inappropriate workarounds.
Author: Sean Kvingedal (FuseChange.org)
I am developing an open source technology to coordinate tens of thousands of social impact projects. The goal is to collectively address complex systemic problems using fewer resources and generating a greater impact by coordinating activities. Ultimately, with a goal to accelerate social change. My hypothesis is that organizations dedicated to social and environmental impact are more likely to collaborate when they can do so seamlessly. This requires participants to easily identify who is doing what, where, when, why, and how, without extensive time-based efforts. They should not have to think about how to collaborate; instead, opportunities should automatically surface, supporting the development of shared goals, knowledge and mutual understanding among participating entities. The core challenge is obtaining the minimum data required to connect and align projects within their local to global ecosystems. In addition, while humans naturally seek collaboration, self-interests and time often become barriers to large-scale collaborative endeavors. There are three components:
Data Capture: We will create open-source tools that are inclusive, offering immediate value for contributed data by automatically connecting projects to the resources they require to succeed. The data itself becomes the foundation to align projects into their systems and ecosystems as a global project repository.
Facilitation Tools for Community Collaboration: Open-source facilitation toolkits are provided to empower communities to collaborate and identify root problems inside their system. Inclusive collaboration is crucial for systems change and communities need tools that break down common social barriers, while enabling anyone to convene and facilitate collaboration.
Virtual Collaboration and Resource Sharing: For communities facing or working on similar challenges, open-source technologies will facilitate ongoing collaboration and resource sharing across projects. These technologies will support shared goals inside a community, across-communities, and across-organizations virtually. The critical aspect of this initiative is to establish a “collaborative systems change movement.” A movement is essential for working on systems change and to collect the necessary data. More importantly, this movement must remain open and decentralized, without ownership by any single entity, which helps to ensure broad participation. In summary, this project seeks to establish an inclusive platform that captures and updates data on social impact projects, facilitating the identification of collaborative opportunities and resource sharing.
We begin with an open-source AI solution that allows social impact organizations and community groups to input their project data, automatically connecting them to the necessary resources. This approach ensures that the data provided is valuable while also generating relational coordination across project activity. Future project data is also captured to start understanding a system's trajectory. Moreover, leveraging AI to recognize patterns across projects will visualize how an array of projects work as a formula to accelerate systems change based on their collective shared impact objectives. I acknowledge that collaboration is inherently challenging. However, making the process of identifying collaborative opportunities seamless can benefit us all. Through open-source technology and AI, we aim to foster a self-sustaining movement that enhances our collective ability to see the whole picture to solve complex social and environmental problems.
Authors: Anthony Cheng (Oregon Health and Science University), Brian Park (Oregon Health and Science University), Shannon Williams (Oregon Health and Science University), Eva Wong (Oregon Health and Science University), and Hans VanDerSchaff (Oregon Health and Science University)
Context: Since the COVID-19 pandemic, access to digital healthcare has become an increasingly important driver of health and equity. Healthcare systems can worsen inequity as program design, implementation, and evaluation are often done without input from communities most affected by systemic oppression. This tends to benefit the dominant culture and/or majority groups and may widen existing power imbalances. Furthermore, health systems have committed historical and ongoing extraction against groups experiencing systematic oppression that emphasizes transactions over relationships. New ways of relating design, power, and social justice are needed. The Community-Led Equity by Design (CO-LED) program was developed to build trust and collaboration between the health system and community-based organizations (CBOs) to forge a patient/community partnership in co-creating health programs with an equity lens in which those most impacted by inequities are positioned as leaders in creating the solutions.
Methods: We recruited local CBOs serving systematically harmed populations experiencing digital health inequities; including Black, Latine, Micronesian Islander, Native American, immigrants, and refugees; to collaborate with a team of clinicians, researchers, and community health workers from Oregon Health and Science University (OHSU). Each CBO identified 1-2 “liaisons” to attend monthly CO-LED meetings and represent the population(s) served by their organization. We used Human-Centered Design (HCD) to facilitate the process of relationship building and power sharing, which mutually reinforced open communication and enhanced the co-creation process. HCD is an approach to designing services, products, and experiences that centers human experiences throughout the design process. Participants interviewed their organizations’ community members to understand their problems, brainstormed solutions, and tested prototypes of potential solution ideas. Qualitative in-depth interviews were carried out with the community liaisons after the project year. Interviewees were asked about their reasons for participating and the value of participating in CO-LED to their organization and community.
Key Findings: Seven CBOs partnered with OHSU CO-LED and engaged for the entire project. Findings from interviews with CBO liaisons emerged in three thematic categories: reflections on building restorative trust; feedback on the facilitation approach; and the individual, organizational, and community influences CO-LED had on CBOs. Some participants developed enduring programs. For example, one CBO collaborated with the education arm of their organization to create a digital skills course. Others invited community members to join culturally specific tutorials on setting up and using a patient health portal or created youth-led digital literacy programs to deliver in senior homes. Liaisons also shared ideas for improvement for future iterations of CO-LED, including ways to improve communication, increase engagement, and set up CBO liaisons to achieve their desired goals.
Takeaways: CO-LED was valued by CBOs as an approach to collaboration between the health system and communities, with positive outcomes toward our collective goals. Trusting health system-CBO relationships were developed, HCD was found to be an effective mode of facilitation, and the partnership led to new community programs. The CO-LED model will be adapted based on these findings and will become an ongoing OHSU program to address issues related to population health inequities beyond digital health.
In times of complex change, leaders can help diverse stakeholders to “see the whole together.” Doing so requires systems thinking, which, according to Peter Senge: “...is a discipline for seeing wholes. It is a framework for seeing interrelationships rather than things, for seeing ‘patterns of change’ rather than static ‘snapshots.’”
Relational leaders help diverse stakeholders to see the whole together while addressing the fundamental human need for connection. According to Otto Scharmer: “The business that leaders are in today is the business of transforming awareness… There is a deep longing for more meaning, for connections.” Mary Parker Follett argued earlier that: “It is impossible . . . to work most effectively at coordination until you have made up your mind where you stand philosophically in regard to the relation of parts to wholes.”
In this panel, leaders from multiple sectors reflected on the challenges and opportunities they are facing, and how they are navigating those challenges and opportunities as relational leaders.


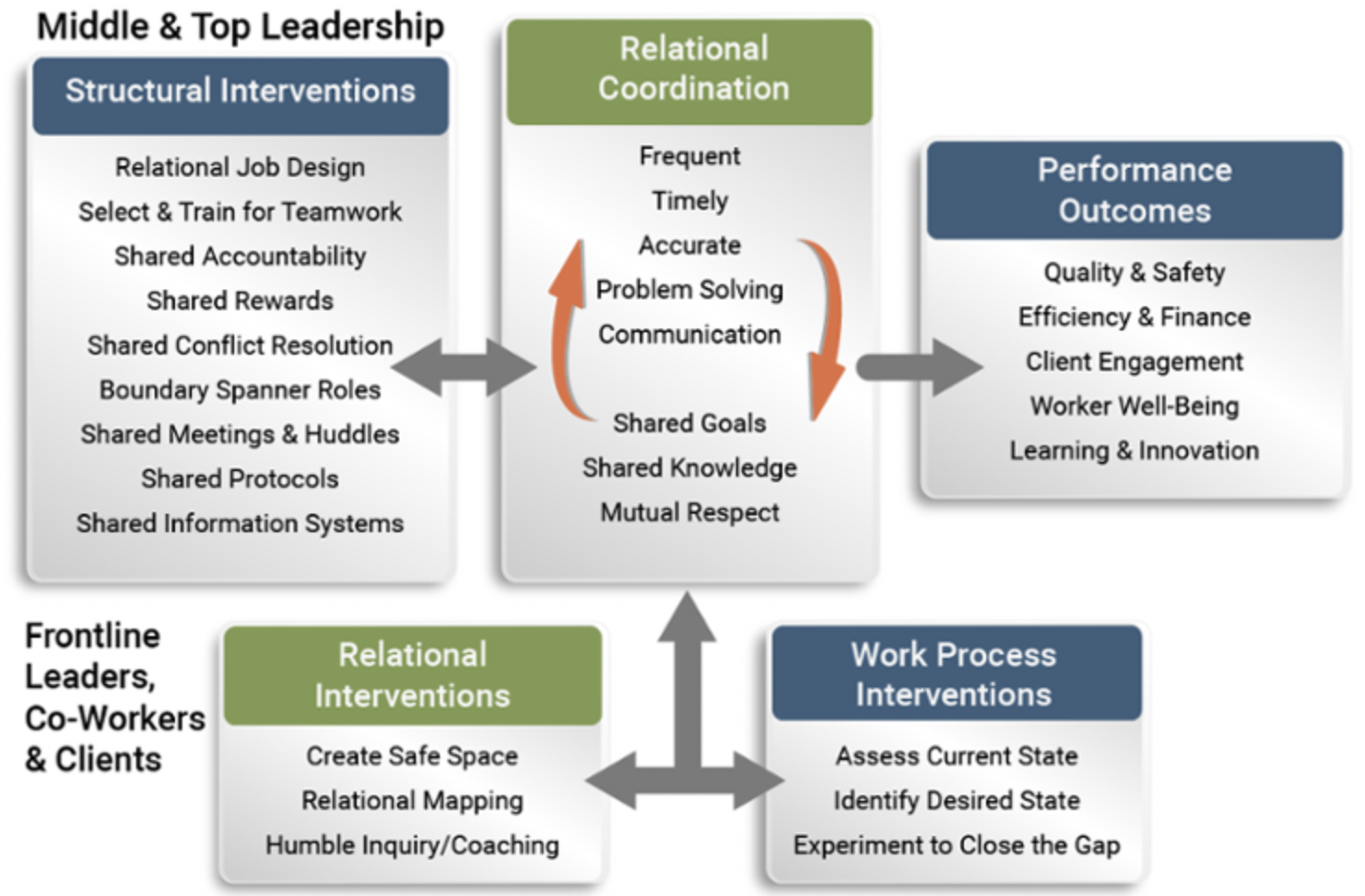








 After the Leadership Panel we celebrated and reflected on a full day of learning at a reception sponsored by
After the Leadership Panel we celebrated and reflected on a full day of learning at a reception sponsored by 




