Hospitalization During Pregnancy Among Pregnant Women with Intellectual and Developmental Disabilities

Introduction
Women with intellectual and developmental disabilities, or IDD, face significant health and socioeconomic disparities during pregnancy and childbirth. Pregnant women with IDD tend to be younger and less educated than their counterparts without disabilities and are less likely to be married.1,2 They are also more likely to use public health insurance and to smoke during pregnancy.1,2 Furthermore, mothers with IDD are at an increased risk for complications during pregnancy, including pre-eclampsia, hypertension, premature labor, venous thromboembolism, and peripartum hemorrhage.1,2,3,4,5 To identify some of these disparities between the pregnancy experiences of women with and without intellectual disabilities, we conducted a study of pre-childbirth hospitalizations among women with and without IDD using the Massachusetts Pregnancy to Early Life Longitudinal Data System (PELL).
Methods
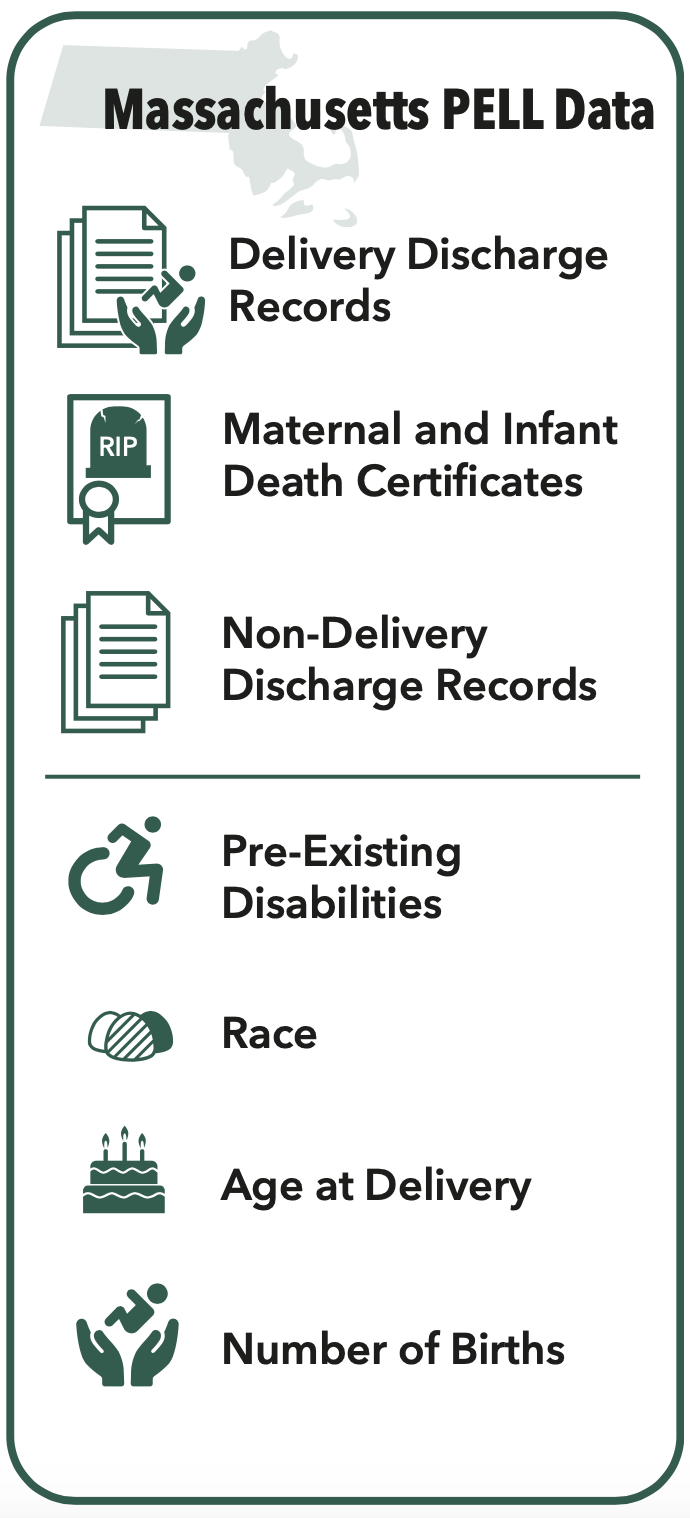
This study used the Massachusetts Pregnancy to Early Life Longitudinal Data System (PELL). PELL is an anonymized database that links all Massachusetts hospital deliveries with delivery discharge records, death certificates of children and their mothers, and non-birth hospital discharge records. PELL lists a number of factors affecting pregnant women and their children during and after pregnancy, including pre-existing disabilities, race, age at delivery, and the number of children women have given birth to. For the purposes of this study, we matched women with IDD and their counterparts without IDD by age at delivery, the year of delivery, and the number of children they already had.
We used the disability criteria listed in PELL to identify women with IDD. These conditions included intellectual disability at all ranges of severity, cerebral palsy, autism, Down syndrome, fragile X syndrome, childhood disintegrative disorder, fetal alcohol syndrome, Rett syndrome, Prader-Willi syndrome, and cri du chat.
We compared emergency department visits, observational hospital stays, and non-delivery hospital stays of women with IDD against those of their non-disabled counterparts. In addition, we considered a number of demographic indicators for this study, including maternal age, education, race or ethnicity, marital status, smoking, and health insurance. We also accounted for medical conditions and disabilities other than intellectual or developmental disabilities, including psychiatric disabilities, diabetes, high blood pressure, seizure disorders, and uterine bleeding.
Results and Discussion
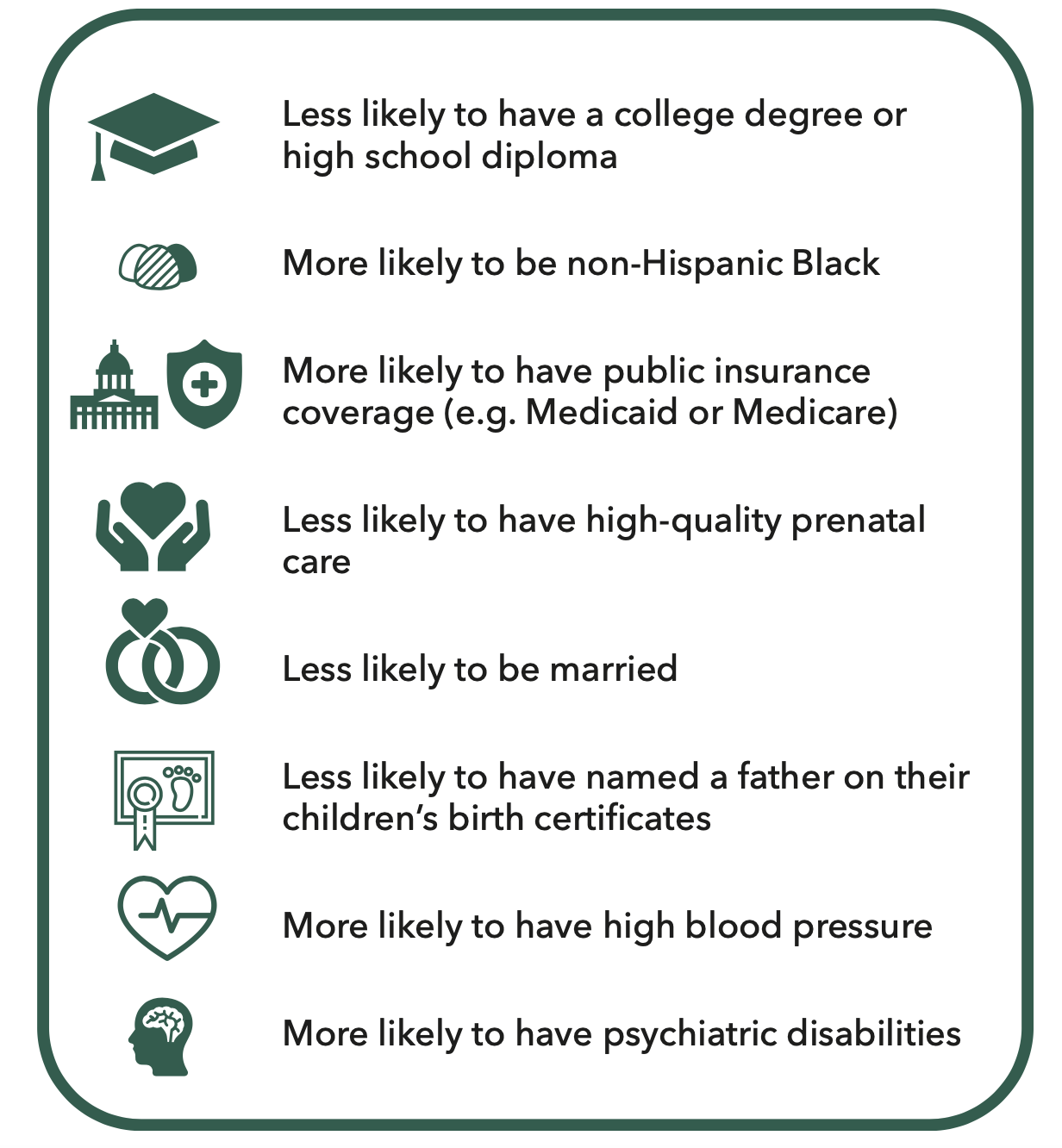
Compared to women without IDD, women with IDD in our study experienced significant socioeconomic and health disparities, and were more likely to be from marginalized groups. Specifically, they were:
- Less likely to have a college degree or high school diploma
- More likely to be non-Hispanic Black
- More likely to have public insurance coverage (e.g. Medicaid or Medicare)
- Less likely to have high-quality prenatal care
- Less likely to be married
- Less likely to have named a father on their children’s birth certificates
- More likely to have high blood pressure
- More likely to have psychiatric disabilities
 Women with IDD were more likely to have emergency department (ED) visits, observational stays, and non-delivery inpatient hospital stays than their counterparts without IDD. During pregnancy, just over half of women with IDD had an ED visit, while about one in three had an observational stay. Almost one-fifth of respondents had a non-delivery stay during pregnancy. In comparison, about one in three women without IDD visited the ED, nearly one-fifth had an observational stay, and 1 in 25 had a non-delivery hospital stay.
Women with IDD were more likely to have emergency department (ED) visits, observational stays, and non-delivery inpatient hospital stays than their counterparts without IDD. During pregnancy, just over half of women with IDD had an ED visit, while about one in three had an observational stay. Almost one-fifth of respondents had a non-delivery stay during pregnancy. In comparison, about one in three women without IDD visited the ED, nearly one-fifth had an observational stay, and 1 in 25 had a non-delivery hospital stay.
We suspect that a number of social, biomedical, and socioeconomic factors contribute to antenatal health disparities among women with intellectual and developmental disabilities. For example, women with IDD receive comparatively little emotional or social support during their pregnancy, and they are less likely to have the robust friend networks that can facilitate good pregnancy outcomes.6,7 Moreover, women with IDD are also likely to have co-occurring psychiatric disabilities and use psychotropic medications (e.g., fluoxetine, risperidone, or duloxetine).8,9 These inequities call for a comprehensive body of research and policy recommendations to improve outcomes for this population.
References
- Höglund, B., Lindgren, P., & Larsson, M. (2012b). Pregnancy and birth outcomes of women with intellectual disability in Sweden: A national register study. Acta Obstetricia et Gynecologica Scandinavica, 91(12), 1381–1387. doi: 10. 1111/j.1600-0412.2012.01509.x
- Mitra, M., Parish, S. L., Clements, K. M., Cui, X., & Diop, H. (2015). Pregnancy outcomes among women with intellectual and developmental disabilities. American Journal of Preventive Medicine, 48(3), 300–308. doi: 10.1016/j. amepre.2014.09.032
- Brown, H. K., Cobigo, V., Lunsky, Y., & Vigod, S. N. (2016). Maternal and offspring outcomes in women with intellectual and developmental disabilities: A population-based cohort study. International Journal of Obstetrics and Gynaecology, 124(5), 757–765. doi: 10.1111/ 1471-0528.14120
- McConnell, D., Mayes, R., & Llewellyn, G. (2008). Women with intellectual disability at risk of adverse pregnancy and birth outcomes. Journal of Intellectual Disability Research, 52(6), 529–535. doi: 10.1111/j.1365-2788.2008. 01061.x
- Parish, S. L., Mitra, M., Son, E., Bonardi, A., Swoboda, P. T., & Igdalsky, L. (2015). Pregnancy outcomes among US women with intellectual and developmental disabilities. American Journal on Intellectual and Develop- mental Disabilities, 120(5), 433–443. doi: 10. 1352/1944-7558-120.5.433.
- Lunsky, Y., & Benson, B. A. (1999). Social circles of adults with mental retardation as viewed by their caregivers. Journal of Developmental and Physical Disabilities, 11(2), 115–129.
- Potvin, L. A., Brown, H. K., & Cobigo, V. (2016). Social support received by women with intellectual and developmental disabilities during pregnancy and childbirth: An exploratory qualitative study. Midwifery, 37, 57–64. doi: 10.1016/j.midw.2016.04.005
- Cooper, S. A., Smiley, E., Morrison, J., Williamson, A., & Allan, L. (2007). Mental ill-health in adults with intellectual disabilities: Prevalence and associated factors. British Journal of Psychiatry, 190, 27–35. doi: 10.1192/bjp.bp. 106.022483.
- Brown, H. K., Cobigo, V., Lunsky, Y., Dennis, C. L., & Vigod, S. N. (2016). Perinatal health of women with intellectual and developmental disabilities and comorbid mental illness. Canadian Journal of Psychiatry, 61(11).
