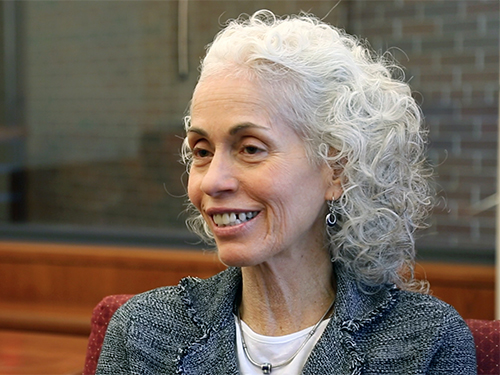
Although the COVID-19 pandemic is now ubiquitous across the United States, public health officials in Los Angeles began fighting the spread far earlier than in most other parts of the country. Chief among them is Heller alumna Barbara Ferrer, PhD’94, director of the Public Health Department for L.A. County. Ferrer was previously the chief strategy officer for the W.K. Kellogg Foundation, and prior to that she served as executive director of the Boston Public Health Commission. She spoke with us about her strategy so far, the immediate challenges her team faces and the path ahead for her community and the nation.
Thank you for taking the time, I know you must be extremely busy right now. That said, I feel compelled to start by asking: How you are doing?
I’m fine, but we’re all extraordinarily tired. For us, this has been going on since January, when we had our first case.
It’s so hard fighting a pandemic with a new virus because the evidence about what we need to do to protect ourselves has changed since we began. When we started, the guidance was that people didn’t need to wear masks. We were convinced that there was little asymptomatic transmission. None of that is true anymore. That’s our reality: being flexible, being able to move quickly as we learn more about the virus.
What are you proudest of in terms of your team’s response to the COVID-19 crisis in L.A. County?
I’m proudest that we’ve never stopped interviewing cases and identifying close contacts. We try to speak with every single identified [COVID-19] case to make sure they know how to appropriately isolate themselves and notify their close contacts about the need to quarantine. We’ve modified our orders so it’s the responsibility of the positive person to notify their close contacts, and we help them figure out what that means. Especially now that this includes people they were in close contact with 48 hours before they were symptomatic.
We interview any high-risk close contacts, which includes people with prior conditions, those who are health care workers, or who live in close congregate housing. We also do investigations at every single institution that has a positive case, which is over 350 institutions now. We follow up at every institution to ensure appropriate testing, isolation of employees and residents who are positive, and quarantine of all close contacts. WE also work with management to implement appropriate infection control and protection for all workers
I think this work makes a big difference, and it only happens because we have an amazing team here
What are your top priorities right now, and how have they changed?
Our top priority is to figure out how to protect people living in institutional settings. There have been huge outbreaks in skilled nursing facilities, outbreaks in shelters for people experiencing homelessness, and outbreaks in prisons and jails. As we move into recovery, we need a plan to protect people who are most vulnerable
Our effort includes offering much more widespread testing of symptomatic and asymptomatic people, especially employees. The residents in nursing homes are usually not able to leave the facilities, so often it’s the employees who are the vector. We required active temperature taking for employees, but it turns out that many asymptomatic people are infectious and spreading the disease in nursing homes. Because so many of the employees are paid relatively low wages and work in two or three different facilities to make ends meet, it is easier for outbreaks to happen in multiple facilities. We need to immediately isolate asymptomatic people if they test positive and all positive people for COVID-19 need to remain in isolation for at least 10 days, including three days of being symptom free if they have symptoms.
Since so few people in L.A. County have been infected with the virus, (about 4% tested positive for antibodies in late April), the vast majority of Angelinos can become infected if exposed. This means that we will need to continue community mitigation and containment for months to come.
What are the key data points you are tracking, and what data do you wish you had that you can’t get?
Every day I look at hospitalizations, ICU and ventilator utilization, and what’s going on with testing, mostly to make sure we’re increasing our testing dramatically. I pay attention to deaths and mortality rates. And I look at the data by race/ethnicity and poverty levels to understand the disproportionality, which we have, and need to take swift action to address and eliminate.
I’d love to have an automatic feed from hospitals, with all info about patients by race and ethnicity, age group, sex, how long they’ve been in the hospital, whether they’re on ventilators. It’d be nice if there were an electronic feed, through a health information exchange or through the state. Right now, it’s difficult: L.A. County has 10 million residents and over 100 hospitals. Not having easy access to electronic health records to do good surveillance has been a limiting factor for us, particularly around disproportionality by race/ethnicity and socioeconomic status. It hinders our ability to do the best job possible. The disproportional deaths among African Americans and Native Hawaiians and Pacific Islanders may be connected to less access to testing and connections with services and care, as well as the increased incidence of chronic diseases; all of these factors are associated with discrimination and racism that manifest through the inequitable distribution of resources needed for optimal health and well-being.
There are growing concerns about the public health and economic costs of delaying primary care, such as vaccinations, cancer screenings and elective surgeries. Have you been able to think long-term about these issues, yet?
Absolutely. You can ask people to delay some routine care for a month, six weeks, but not much longer than that. You don’t want a measles outbreak. By the time we’re in the next flu season, people need their flu shots.Our hospitals are at 50% capacity right now. It’s great that we can surge here if we need to, but you don’t want to keep hospitals with so many empty beds. As long as hospitals can ensure the PPE [personal protective equipment] supply chain, enough staffing, enough routine testing of health care workers and ability to hospitalize people with respiratory illness, we can then relax some of the restrictions for patients and providers to do essential care. We’d still be prepared for a surge that would require quick decompression at hospitals to safely accommodate significant increases in patients. We’re not on the other side of this epidemic yet, but we’ve definitely managed to slow the spread in a good way that allows our system to resume some normal operations while we protect our ability to surge.
You’ve had a long and incredibly successful career, and I’m sure that your Heller PhD feels like a lifetime ago, at this point. That said, do you still rely on anything in particular that you learned at Heller in your work today?
I really appreciate the fact that I gained some important skills on how to use data to inform decisions, while also recognizing there’s always limitations with the data you have, and trying to be creative with looking at different sources of information to help us understand what’s going on. That’s certainly been the case here, with this crisis.
