For Dr. Ihsan Kaadan, MS GHPM’16, serving as a doctor during a major crisis is, sadly, nothing new. In 2012, he completed his first year of residency at Aleppo University Hospital as the Syrian conflict raged on, which eventually forced him to move to the United States to continue his medical training. He earned his MS in International Health Policy in Management at Heller, then did cardiology research for two years at Massachusetts General Hospital before resuming his training. Now, as an internal medicine resident at Boston Medical Center, he’s on the front lines of the COVID-19 epidemic, drawing on his previous experiences to keep him grounded during this challenging time.
What does your typical day look like now, and how are you feeling?
As a second-year internal medicine resident, I’m seeing 100% corona patients right now. I’m working 12-hours shifts, six days a week. Life has completely changed. The type of management we do, the encounters we see, it’s all changed. At the end of the day you’re tired.
We have a clinical word, “active,” to describe patients whose situations are changing. For example, a patient doesn’t need oxygen, then all of a sudden needs a couple of liters. That’s an important sign. In the past, if I was working nights, you might get a few pages per hour while you’re covering 30 patients. Now, you’re getting many more pages. It’s stressful.
My job starts after patients come through the emergency department (ED), which triages and determines who needs to be admitted. Then after that, we get a page from the ED and we get to work.
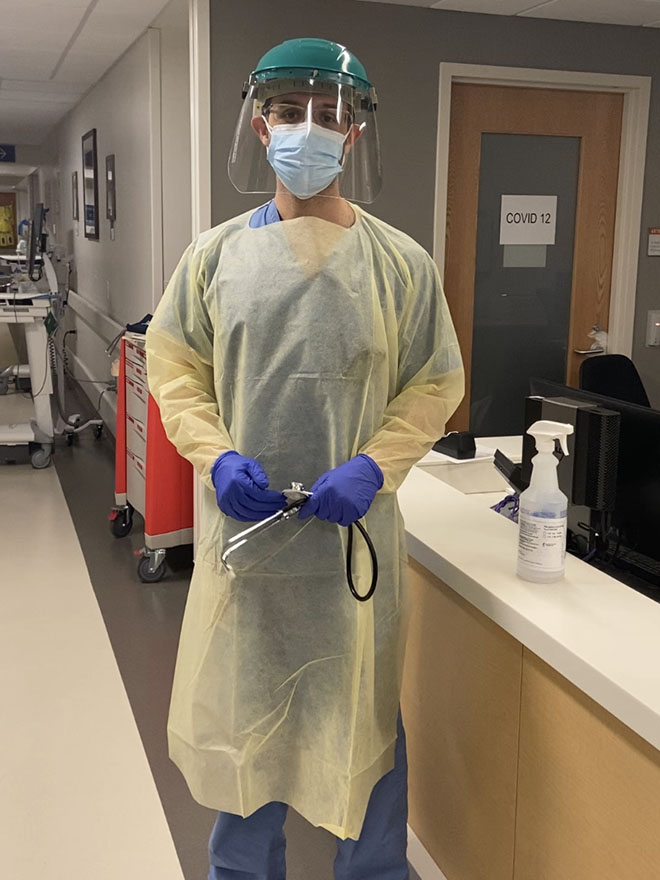
First, I have to make sure the patient is stable, looking at vitals and lab work before I call for sign out. Then I have to go in the room and see the patient once they hit the floor. The challenging part is that you really need to wear PPE [personal protective equipment]. That process takes so long: you have to put the gown on, gloves, face masks and a shield as well. Then I go in to examine them. I’m getting the full story of why they came. Most patients come with cough, fever, body ache, and shortness of breath, and it’s important to ask if they have a sick contact. After that, I develop a plan for treatment.
One of the most important vitals is oxygenation. For patients whose oxygenation goes down, we’ll give them oxygen, then we contact the ICU to prepare them for possible intubation, if their oxygen requirement increases more than certain limit. Two weeks ago, I was working in the ICU, where I had to monitor some patients who were intubated.
You have to be cautious. I’m seeing young people. I have many patients with no known medical history who are coming to the hospital because of corona.
How does your schedule now differ from your typical schedule?
As a regular second-year resident, I would do three weeks inpatient, one week outpatient. We’d rotate in different specialties, like internal medicine, nephrology, cardiology, and do research as well, since this is an academic center.
Now, everything has changed. We’re not seeing any outpatient patients in person anymore. Instead, we call them over the phone. Even subspecialty fellows and attending physicians who have done all their training are working with internal medicine residents and attending COVID patients. For example, you might see pediatric doctors working on adults who have corona. Everyone is working so hard, putting their lives on the front lines.
How did your time in Syria prepare you for working during this pandemic?
I did my first year of residency at Aleppo University Hospital during the conflict. Mentally and physically I’m already prepared for working in a crisis. I don’t feel like this is completely unknown to me. We used to have shortages all the time, with high numbers of patients coming to the hospital. I worked with a lot of people who were displaced, which makes things complicated. I saw a lot of hepatitis; you get Hepatitis A if the water and environment isn’t clean, which happens during a crisis.
I think about what would happen if COVID-19 went to Syria all the time. I hope this pandemic doesn’t go to Syria or other countries that don’t have the infrastructure to deal with such a situation.
How do you draw on your Heller experience today?
I really miss Heller. Before the pandemic, I would sometimes take the bus to campus and just walk around and see Heller.
The skills we learned during MS classes about health systems strengthening and some of the elements that make this health system fragile—you think about those things all the time during a pandemic. When you read about the statistics around corona, I’m using the knowledge from epidemiology to really understand what those numbers mean.
To the Heller community, I want to say that you guys are really in my thoughts. I hope everyone is safe. Take advantage of this time that you’re staying home to spend it with your family. I want to see people go back to campus and celebrate the end of the pandemic together one day soon.
